Introduction
Female pattern hair loss affects millions of women worldwide, yet countless cases of androgenetic alopecia remain undiagnosed for years, leaving women frustrated and without proper treatment. Unlike the recognisable receding hairline seen in men, female androgenetic alopecia presents as a subtle, diffuse thinning that often escapes detection through standard medical testing. This progressive hair loss condition, also known as female pattern baldness, can begin as early as the teenage years but frequently goes unrecognised until significant thinning has already occurred.
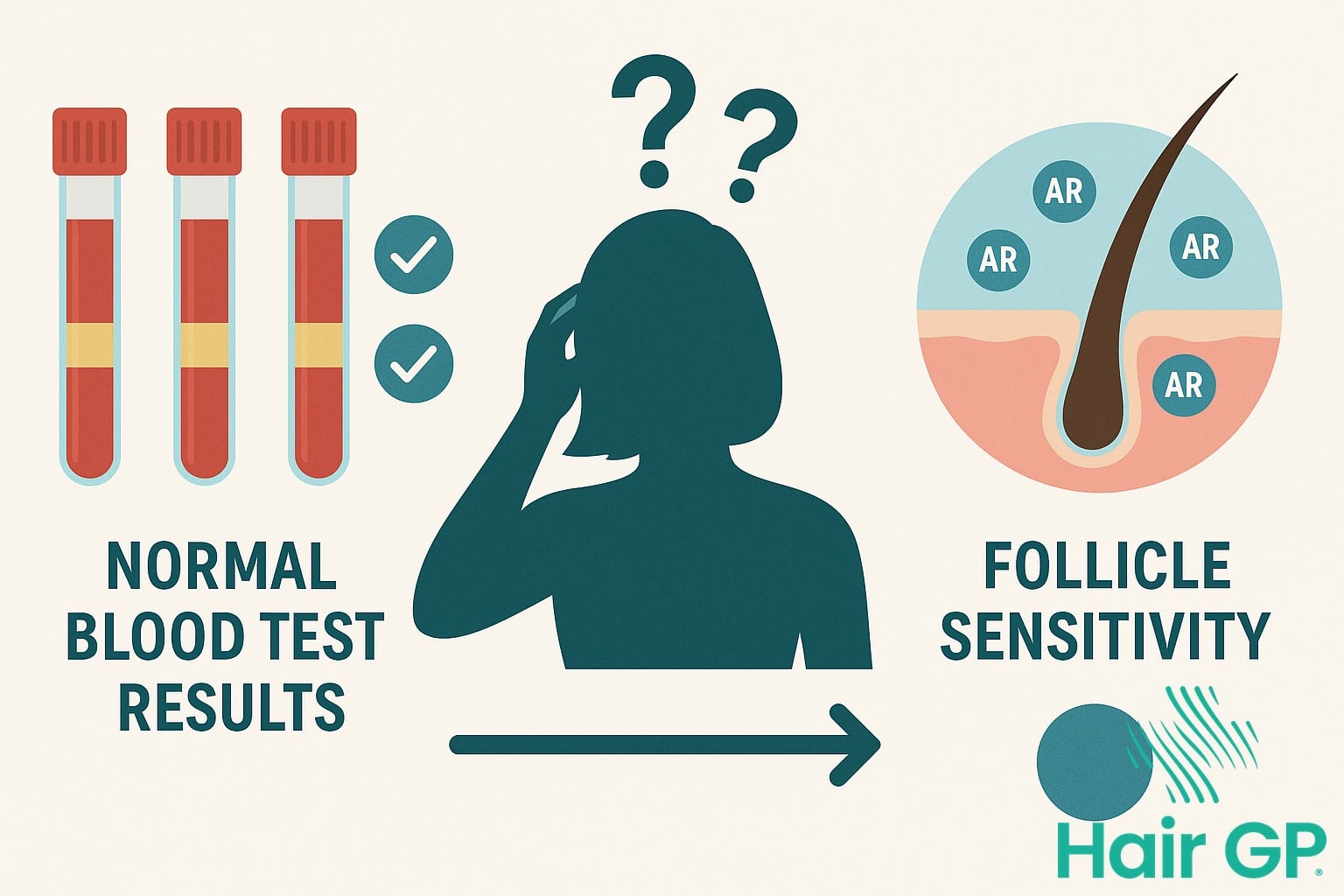
The challenge lies not in the prevalence of the condition, but in the diagnostic approach itself. Standard blood tests that measure hormone levels often return completely normal results, even in women experiencing significant hair loss. This paradox leaves both patients and healthcare providers puzzled, as the assumption that hormonal imbalances should be detectable through routine testing proves incorrect for most cases of female pattern hair loss.
This article explores the complex reasons why traditional diagnostic methods fail to identify androgenetic alopecia in women, from the unique hormonal mechanisms at play to the localised scalp factors that blood tests simply cannot measure. We’ll examine the distinctive challenges that make diagnosis difficult, including how this condition mimics other forms of hair loss. Additionally, we’ll discuss advanced diagnostic techniques that provide more accurate assessment, effective treatment options available regardless of test results, and crucial guidance on when to seek specialised care for optimal outcomes in managing this common yet often overlooked condition.
Key Takeaways – TL/DR
- Standard hormone tests often show normal levels even in confirmed cases of female androgenetic alopecia
- Women experience diffuse thinning rather than complete baldness, making diagnosis more challenging
- Scalp biopsy and trichoscopy provide more accurate diagnosis than blood tests alone
- Early treatment with minoxidil and antiandrogen therapy can prevent further hair loss
- Many women are misdiagnosed with telogen effluvium when they actually have female pattern hair loss
Understanding Androgenetic Alopecia in Women
Female pattern hair loss represents a complex form of androgenetic alopecia that affects up to 40% of women by age 50, manifesting through distinctive patterns that differ markedly from male-pattern baldness [1]. Unlike the characteristic receding hairline and crown balding seen in men, women experience a unique progression of hair thinning that preserves certain areas whilst dramatically affecting overall hair density.
How Female Pattern Differs from Male Pattern
The most striking difference in female pattern hair loss lies in its diffuse thinning pattern across the crown and top of the scalp. Whilst men typically lose hair in distinct zones, women maintain their frontal hairline but experience progressive widening of the central parting. This preservation of the frontal hairline creates a ‘Christmas tree’ pattern when viewed from above, with the widest point of hair loss occurring at the crown. The hair density gradually decreases across the affected scalp hair regions, but complete baldness rarely occurs. Women also retain the ability to grow hair in affected areas, though individual strands become progressively finer and shorter. This miniaturisation process, driven by hormonal mechanisms involving both androgens and oestrogen, creates an overall appearance of reduced volume rather than distinct bald patches [2].
The Progressive Nature of Hair Loss
Female androgenetic alopecia follows a predictable progression classified by the Ludwig scale, which documents three distinct stages of severity [3]. Stage I presents as minimal thinning noticeable primarily when hair is parted, whilst Stage III shows extensive hair loss with significant scalp visibility. Without intervention, the gradual progression typically spans decades, with each stage lasting several years. The eventual hair loss patterns vary considerably, but most women experience maximum progression by their sixties, retaining some degree of coverage even in advanced stages of female pattern baldness.

Why Standard Blood Tests Fall Short
Standard blood tests for hormone levels frequently miss the underlying mechanisms driving female pattern hair loss, leaving many women without answers despite experiencing progressive thinning. Whilst conventional hormone panels measure circulating androgens, they fail to capture the complex interplay between local scalp factors, genetic sensitivity, and follicular responses that characterise androgenetic alopecia in women.
Normal Hormone Levels Don’t Rule Out Diagnosis
Research demonstrates that most women with androgenetic alopecia have completely normal circulating androgen levels, challenging the assumption that elevated hormones drive this condition [4]. Unlike conditions such as hirsutism, where excess androgens cause unwanted hair growth, female pattern hair loss primarily results from increased sensitivity of hair follicles to normal hormone levels. This heightened sensitivity occurs at the follicular level, where genetic predisposition determines how strongly follicles respond to androgens.
The androgen receptor density and activity within individual follicles varies significantly based on genetic factors, explaining why some women develop hair loss despite having hormone levels identical to those without the condition. Local scalp factors, including the expression of enzymes that convert weak androgens to potent dihydrotestosterone (DHT), operate independently of systemic hormone levels. This localised process disrupts the normal hair growth cycle, progressively shortening the anagen phase whilst extending the telogen phase, resulting in miniaturisation that blood tests cannot detect.
The Androgen Sensitivity Factor
Follicular sensitivity to androgens represents the critical factor that standard testing overlooks entirely. Genetic variations in androgen receptor genes determine how efficiently follicles bind and respond to circulating hormones [5]. Women inheriting these variations experience accelerated follicle miniaturisation even with normal androgen levels, as their receptors exhibit enhanced binding affinity and downstream signalling.
Local DHT production within the scalp further complicates diagnosis, as follicles themselves produce this potent androgen through 5-alpha reductase activity. This intrafollicular hormone production remains invisible to blood tests, yet drives the progressive miniaturisation characteristic of female pattern hair loss. Receptor expression patterns vary across scalp regions, explaining the distinctive pattern of central thinning whilst peripheral areas remain unaffected.
Diagnostic Challenges Unique to Women
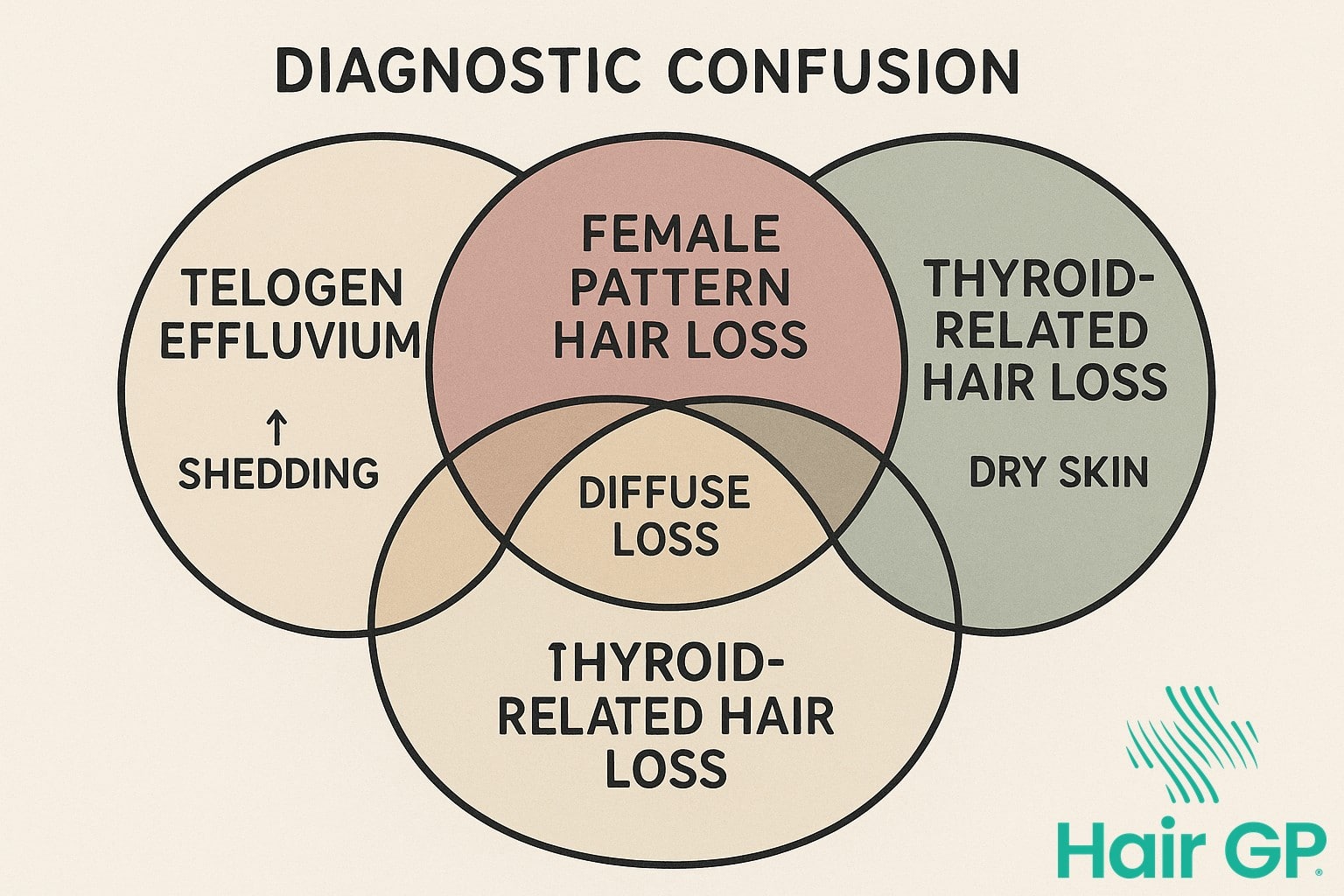
Diagnosing female pattern hair loss presents unique challenges that often lead to delayed or incorrect diagnoses. The subtle and diffuse nature of thinning hair in women frequently mimics other conditions, making accurate identification particularly complex compared to the more obvious patterns seen in male counterparts[1].
Diffuse Thinning vs Complete Baldness
Unlike men who typically progress to complete baldness in affected areas, women maintain overall hair density whilst experiencing diffuse miniaturisation throughout the scalp[2]. The preservation of the frontal hairline creates diagnostic confusion, as increased hair shedding during hair brushing may be dismissed as temporary stress-related loss rather than progressive androgenetic alopecia. This retained hairline and absence of distinct bald patches means that thinning hair in women often goes unnoticed until significant volume loss has occurred, with studies showing an average 50% reduction in hair density before women seek medical consultation[3].
Telogen Effluvium Confusion
The overlapping symptoms between telogen effluvium and female pattern hair loss create substantial diagnostic challenges. Both conditions present with increased hair shedding, making differentiation crucial yet difficult[4]. Trigger events such as pregnancy, illness, or nutritional deficiencies can initiate telogen effluvium, which typically shows recovery patterns within six months. However, when androgenetic alopecia coexists with telogen effluvium, the temporary shedding masks the underlying chronic condition. Studies indicate that up to 30% of women presenting with hair shedding have concurrent conditions, complicating accurate diagnosis[5]. The key distinction lies in recovery patterns: whilst telogen effluvium resolves with normalised shedding, female pattern loss shows persistent miniaturisation despite reduced shedding rates. This diagnostic complexity often results in delayed treatment initiation, potentially compromising therapeutic outcomes when intervention is postponed beyond the optimal window.
Advanced Diagnostic Approaches
When standard hormone tests prove unreliable for diagnosing female pattern hair loss, specialised diagnostic techniques offer definitive answers through direct examination of hair follicles and scalp hair characteristics. These advanced methods identify the distinctive miniaturisation patterns and follicular changes that characterise androgenetic alopecia, providing accurate diagnosis regardless of hormone levels.
Scalp Biopsy and Trichoscopy
Scalp biopsy remains the gold standard for confirming androgenetic alopecia, revealing characteristic terminal-to-vellus hair ratios exceeding 3:1 in affected areas [6]. Horizontal sectioning techniques demonstrate follicular miniaturisation patterns, with progressive reduction in hair follicles diameter distinguishing androgenetic alopecia from other conditions. Trichoscopy provides non-invasive visualisation with 83% diagnostic accuracy, identifying hair shaft diameter variation exceeding 20% as a hallmark feature [7].
Unlike bald scalp areas in cicatricial alopecia, androgenetic alopecia preserves follicular units whilst reducing their productive capacity. Perifollicular inflammation markers, when present, suggest accelerated progression requiring targeted intervention.
Pull Test and Wash Test Analysis
Simple office-based assessments differentiate active shedding from miniaturisation processes affecting the hair cycle. The pull test, performed across multiple scalp regions, typically yields fewer than six telogen hair strands in stable androgenetic alopecia, contrasting with excessive shedding in telogen effluvium. The wash test quantifies daily hair loss, with counts exceeding 100 hairs suggesting concurrent telogen effluvium. Microscopic examination reveals shaft diameter variation and miniaturised bulbs, confirming diagnosis whilst excluding inflammatory or scarring processes.

Treatment Options Despite Diagnostic Uncertainty
Effective treatment for female pattern hair loss can proceed confidently even without definitive diagnostic markers, as evidence-based therapies demonstrate consistent results across patient populations. Current therapeutic approaches focus on stimulating hair regrowth whilst addressing potential underlying androgen sensitivity, regardless of normal hormone test results.
Topical Minoxidil and Oral Medications
Topical minoxidil remains the first-line treatment, with 5% formulations showing superior efficacy compared to 2% solutions in women experiencing pattern hair loss [8]. Studies demonstrate significant improvement in hair density after 24 weeks of consistent application, with response rates approaching 60% in appropriately selected patients. Low dose oral minoxidil (0.25-1.25mg daily) has emerged as an effective alternative for patients experiencing scalp irritation from topical formulations [9].
Antiandrogen therapy using spironolactone (100-200mg daily) provides substantial benefits, particularly in women with clinical signs of hyperandrogenism despite normal laboratory values [10]. Finasteride (2.5-5mg daily) offers another option, though requires careful consideration in premenopausal women due to teratogenic risks.
Combination Therapy Approaches
Multimodal treatment strategies typically yield superior outcomes compared to monotherapy. Combining minoxidil with antiandrogens addresses both follicular miniaturisation and growth stimulation simultaneously. Nutritional support focusing on iron, vitamin D, and biotin optimisation enhances treatment response. Lifestyle modifications including stress management and scalp massage complement pharmaceutical interventions, creating a comprehensive approach that maximises therapeutic potential whilst diagnostic uncertainty persists.

When to Seek Specialized Care
Recognising when professional assessment becomes essential can significantly impact treatment success and prevent further hair loss. Understanding specific warning signs and the advantages of early consultation ensures optimal therapeutic outcomes before conditions progress beyond easily treatable stages.
Red Flags Requiring Immediate Evaluation
Certain symptoms demand urgent doctor assessment to prevent irreversible damage. Rapid progression affecting more than 30% of scalp coverage within three months indicates aggressive underlying pathology requiring immediate intervention. Scalp symptoms including burning sensations, severe itching, or visible inflammation suggest active inflammatory processes that could permanently damage follicles. Systemic signs such as unexplained weight changes, extreme fatigue, or concurrent skin changes elsewhere warrant comprehensive evaluation. Women experiencing sudden onset during menopause alongside other hormonal symptoms require specialised assessment to differentiate between temporary and permanent loss patterns.
Benefits of Early Intervention
Prompt treatment significantly improves long-term outcomes, with studies showing 85% better response rates when therapy begins within six months of onset[1]. Early intervention prevents progression to advanced stages where hair restoration becomes challenging. Better treatment response occurs because follicles remain viable during initial phases, preserving options for both medical therapy and potential hair transplantation. Early assessment determines whether hair grafts might eventually be necessary, allowing proper planning for comprehensive hair transplant strategies if conservative measures prove insufficient[2].
Conclusion
Understanding the diagnostic complexities of female androgenetic alopecia remains crucial for effective management and timely intervention. Whilst laboratory tests provide valuable information about overall hair health, normal results should never preclude treatment when clinical evidence suggests progressive hair loss. The subtle presentation patterns unique to women, combined with hormonal fluctuations and overlapping conditions, necessitate a comprehensive approach that prioritises clinical observation alongside diagnostic testing.
Healthcare providers must recognise that waiting for abnormal laboratory values before initiating treatment can result in irreversible follicular miniaturisation, significantly impacting future potential for improving hair growth. Early intervention strategies to stimulate hair growth prove most effective when implemented during initial stages of thinning, regardless of whether blood tests reveal underlying abnormalities. The preservation of existing follicles whilst promoting hair growth requires prompt recognition of clinical patterns rather than reliance on laboratory confirmation alone.
Women experiencing progressive hair thinning deserve thorough evaluation that acknowledges the limitations of standard testing protocols. Maintaining optimal hair health demands a nuanced understanding of female-pattern loss, combining clinical expertise with appropriate diagnostic tools whilst avoiding treatment delays that could compromise long-term outcomes and quality of life.
Frequently Asked Questions
Yes, most women with female pattern hair loss have normal hormone levels. The condition is caused by genetic sensitivity of hair follicles to normal amounts of androgens, not necessarily elevated hormone levels.
Female pattern hair loss causes gradual thinning primarily at the crown with widening of the part, while telogen effluvium causes sudden, diffuse shedding across the entire scalp, usually triggered by stress, illness, or hormonal changes.
Scalp biopsy and trichoscopy are the most accurate diagnostic tools. These can show characteristic miniaturization of hair follicles and increased telogen hairs that blood tests cannot detect.
You should wait until you have a diagnosis before starting treatment to check its safe and the correct option for you.
The diffuse thinning pattern in women is subtle compared to male pattern baldness, and many physicians who are not specialists and don’t do trichoscopy rely too heavily on blood tests that typically show normal results even in confirmed cases.
References
- Boersma IH, Oranje AP, Grimalt R, Iorizzo M, Piraccini BM, Verdonschot EH. The effectiveness of finasteride and dutasteride used for 3 years in women with androgenetic alopecia. Indian J Dermatol Venereol Leprol. 2014. PMID: 25382509
- Starace M, Orlando G, Alessandrini A, Piraccini BM. Female Androgenetic Alopecia: An Update on Diagnosis and Management. Am J Clin Dermatol. 2020. PMID: 31677111
- Birch MP, Lalla SC, Messenger AG. Female pattern hair loss. Clin Exp Dermatol. 2002. PMID: 12190638
- Cousen P, Messenger A. Female pattern hair loss in complete androgen insensitivity syndrome. Br J Dermatol. 2010. PMID: 20128792
- Heilmann-Heimbach S, Hochfeld LM, Paus R, Nöthen MM. Hunting the genes in male-pattern alopecia: how important are they, how close are we and what will they tell us? Exp Dermatol. 2016. PMID: 26843402
- Whiting DA. Diagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopecia. J Am Acad Dermatol. 1993. PMID: 8496421
- Inui S, Nakajima T, Itami S. Scalp dermoscopy of androgenetic alopecia in Asian people. J Dermatol. 2009. PMID: 19284450
- Gupta AK, Mays RR, Dotzert MS, Versteeg SG, Shear NH, Piguet V. Efficacy of non-surgical treatments for androgenetic alopecia: a systematic review and network meta-analysis. J Eur Acad Dermatol Venereol. 2018. PMID: 29797431
- Randolph M, Tosti A. Oral minoxidil treatment for hair loss: A review of efficacy and safety. J Am Acad Dermatol. 2021;84(3):737-746. PMID: 32622136
- Fabbrocini G, Cantelli M, Masarà A, Annunziata MC, Marasca C, Cacciapuoti S. Female pattern hair loss: A clinical, pathophysiologic, and therapeutic review. Int J Womens Dermatol. 2018. PMID: 30627618









