Introduction
Trichotillomania, a complex hair pulling disorder that affects millions of people worldwide, can feel like an insurmountable challenge for those caught in its grip. This compulsive hair pulling disorder goes far beyond a simple habit – it’s a recognised mental health condition that can significantly impact daily life, self-esteem, and relationships. Despite its prevalence, many individuals struggle in silence, unaware that effective recovery strategies exist.
If you’re living with trichotillomania, you’re not alone. This condition, classified among body focused repetitive behaviors, affects people of all ages and backgrounds. The compulsive urge to pull out hair from the scalp, eyebrows, eyelashes, or other body areas can feel overwhelming, but understanding is the first step towards breaking free from this cycle.
This comprehensive guide explores the multifaceted nature of recovery from hair pulling behavior. We’ll delve into what drives these urges, examining the emotional and environmental factors that trigger pulling episodes. You’ll discover evidence-based professional treatments that have helped countless individuals regain control, alongside practical coping strategies you can implement in your daily life. We’ll also navigate the recovery process itself, acknowledging both the challenges and victories along the way.
Recovery from trichotillomania is possible. While the journey may not always be linear, with the right knowledge, support, and tools, you can break the hair-pulling cycle and reclaim your life. Let’s explore how to transform your relationship with this condition and build a future free from its constraints.
Key Takeaways – TL/DR
- Trichotillomania is a treatable impulse control disorder affecting 1-2% of the population
- Habit reversal therapy and cognitive behavioural therapy show 60-80% success rates
- Recovery requires identifying triggers, developing coping strategies, and practicing self-compassion
- Hair regrowth is possible with consistent treatment and reduced pulling behaviour
- Professional support combined with self-help techniques yields the best outcomes
Understanding Trichotillomania
Understanding trichotillomania begins with recognising it as a legitimate impulse control disorder affecting approximately 1-2% of the population[1]. Classified within body focused repetitive behaviors alongside skin picking and nail biting, this condition involves recurrent hair pulling that results in noticeable hair loss despite repeated attempts to stop[2].
Recognising Symptoms and Warning Signs
Trichotillomania symptoms extend beyond the visible hair loss patterns. The repeated pulling behaviour typically occurs during periods of stress or relaxation, with individuals experiencing mounting tension before pulling and temporary relief afterwards. Physical indicators include bald patches, thinning areas, or unusual hair growth patterns. Emotional distress indicators encompass shame, anxiety, and significant functional impairment in social or occupational settings.
The Connection to OCD and Related Disorders
While distinct from obsessive compulsive disorder, trichotillomania shares notable similarities and comorbidity rates of approximately 26% with OCD[3]. Both conditions involve repetitive behaviours, though hair pulling lacks the obsessional thoughts characteristic of OCD. Strong correlations exist with other body focused repetitive behaviors, particularly skin picking disorder and compulsive nail biting, suggesting shared neurobiological mechanisms underlying these impulse control disorders.

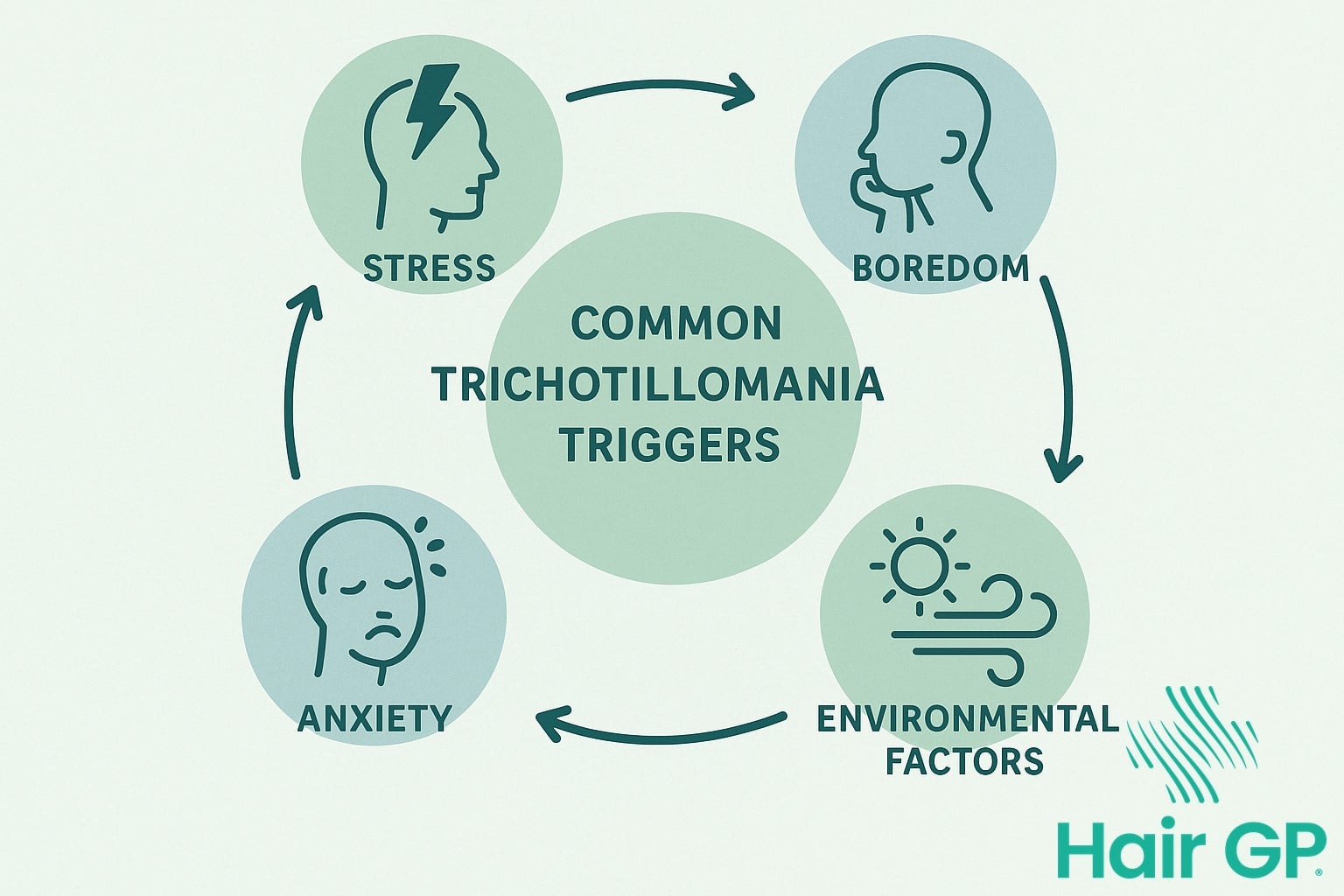
Common Triggers and Patterns
Understanding your personal hair pulling triggers is crucial for managing trichotillomania. Most people who pull hair experience specific patterns linked to emotional states, environments, or activities. Common hair pulling triggers include stress from work or relationships, feelings of anxiety or boredom, and quiet moments when hands are idle. Many individuals notice increased hair pulling urges whilst watching television, reading, or working at a computer.
Environmental factors play a significant role to. Certain locations like your bedroom, bathroom, or car might become associated with pulling hair behaviours. Recognising these patterns helps you anticipate when urges might arise. Some people experience stronger impulses during specific times of day, particularly in the evening when fatigue sets in.
To effectively stop hair pulling, start by keeping a simple diary noting when and where trichotillomania pull episodes occur. This awareness forms the foundation for developing personalised intervention strategies that work for your unique situation.
Evidence-Based Treatment Approaches
Evidence-based treatment approaches offer hope for individuals struggling with trichotillomania, with scientifically proven methods demonstrating significant effectiveness in managing this complex condition. Professional interventions including habit reversal therapy, cognitive behavioural therapy, and acceptance and commitment therapy have shown measurable success rates, providing structured pathways to recovery through implementation of targeted therapeutic strategies.
Habit Reversal Training Explained
Habit reversal training (HRT) stands as the gold-standard trichotillomania treatment, with studies showing 68% of participants achieving significant improvement [4]. This comprehensive approach begins with awareness training, helping individuals recognise triggers and early warning signs before pulling occurs. Competing response practice forms the cornerstone of HRT, teaching patients to engage alternative behaviours when urges arise – such as clenching fists or manipulating stress balls. Social support systems strengthen treatment outcomes, with family members and friends learning to provide encouragement without enabling the behaviour.
CBT and ACT for Trichotillomania
Cognitive behavioural therapy addresses the thought patterns underlying hair pulling, helping patients identify and modify distorted thinking that perpetuates the behaviour. Acceptance and commitment therapy takes a different approach, encouraging individuals to accept uncomfortable urges whilst committing to value-based actions [5]. Mindfulness techniques integrated within these therapies enhance present-moment awareness, reducing automatic pulling episodes and improving overall emotional regulation.
Working with a Therapist
Choosing the right therapist requires seeking professionals experienced in body-focused repetitive behaviours. During initial consultations, discuss their familiarity with habit reversal therapy and evidence-based approaches. Treatment planning should include clear goals, regular progress assessments, and flexibility to adjust strategies as needed for optimal outcomes.
Developing Healthy Coping Strategies
Developing effective coping strategies forms the cornerstone of managing trichotillomania successfully. When urges arise, having readily available alternatives can make the difference between maintaining control and giving in to hair pulling behaviours. Creating a personalised toolkit begins with identifying sensory substitutes that satisfy the physical need for stimulation. Many individuals find relief through stress balls, fidget toys, or textured fabrics that provide tactile feedback similar to hair manipulation.
To stop trichotillomania effectively, integrating stress management techniques proves essential as anxiety often triggers pulling episodes. Deep breathing exercises, progressive muscle relaxation, and mindfulness meditation serve as powerful coping mechanisms that address underlying tension. These practices help interrupt the automatic response pattern, creating space to choose healthier coping strategies instead of defaulting to hair pulling.
Behavioural replacements offer another pathway to replace hair pulling urges with constructive activities. Engaging hands through creative pursuits like drawing, knitting, or playing musical instruments redirects the physical impulse productively. Some find success with barrier methods such as wearing gloves or bandages on fingertips during high-risk situations. The key to develop healthier coping strategies lies in experimenting with various techniques to discover what resonates personally, building a comprehensive approach that addresses both physical and emotional aspects of the condition.

The Recovery Journey
The recovery journey from trichotillomania involves navigating both physical healing and emotional growth. Understanding realistic expectations for hair regrowth and developing self compassion during setbacks creates a foundation for lasting recovery.
Hair Regrowth and Physical Recovery
Hair growth typically occurs in stages, with initial regrowth appearing as fine, soft hair within 3-4 months after you stop pulling. Hair grows at approximately 1cm per month, though damaged follicles may produce slower or altered growth patterns. Caring for recovering areas involves gentle cleansing, avoiding harsh chemicals, and protecting thinning hair with silk pillowcases or loose hairstyles.
Building Long-Term Success
Sustainable recovery requires developing relapse prevention strategies and maintaining support systems. When urges arise, having alternative activities ready helps redirect the impulse to pull. Celebrating small wins, whether it’s one pull-free day or noticing new hair regrowth, reinforces positive progress. Building connections with support groups or trusted friends provides encouragement during challenging moments, reminding you that recovery is possible.

Conclusion
The journey of trichotillomania recovery requires patience, persistence, and self-compassion. Whilst managing trichotillomania presents unique challenges, countless individuals have successfully overcome this hair pulling disorder through comprehensive treatment approaches and unwavering determination. Recovery isn’t linear—setbacks are normal and don’t diminish your progress or potential for healing.
Professional therapy remains the cornerstone of treating trichotillomania effectively. Whether through cognitive behavioural therapy, habit reversal training, or acceptance and commitment therapy, specialised support provides essential tools for lasting recovery. Combined with personal strategies like mindfulness practices, stress management techniques, and supportive environments, these interventions create a robust foundation for healing.
Remember that seeking help demonstrates strength, not weakness. Every small step towards recovery matters, from reaching out to a therapist to implementing daily coping strategies. Self-compassion throughout this process proves crucial—be gentle with yourself during difficult moments and celebrate each victory, however minor it may seem.
Your recovery journey is unique, and with appropriate support, evidence-based treatment, and personal commitment, overcoming trichotillomania is entirely achievable. The path forward begins with believing in your capacity to heal and taking that first courageous step towards professional help and lasting change.
Frequently Asked Questions
Recovery timelines vary greatly between individuals. While some people see significant improvement within 8-12 weeks of consistent treatment, complete recovery can take months to years. The key is focusing on progress rather than perfection, as even reducing pulling frequency is a valuable achievement.
In most cases, hair will regrow once pulling stops. However, years of repeated pulling can damage hair follicles, potentially leading to permanent hair loss in severe cases. Early intervention and treatment significantly improve the chances of full hair regrowth.
Yes, trichotillomania is often related to anxiety and shares similarities with OCD. It’s classified as a body-focused repetitive behavior and frequently co-occurs with anxiety disorders, OCD, and depression. Many people pull their hair as a way to manage stress or uncomfortable emotions.
Normal hair twirling or playing is typically done without pulling hair out and doesn’t cause distress or hair loss. Trichotillomania involves compulsive pulling that results in noticeable hair loss, significant distress, and difficulty stopping despite negative consequences.
References
- Keuthen NJ, Curley EE, Scharf JM, Woods DW, Lochner C, Stein DJ et al.. Predictors of comorbid obsessive-compulsive disorder and skin-picking disorder in trichotillomania. Ann Clin Psychiatry. 2016. PMID: 27901519
- Stein DJ, Flessner CA, Franklin M, Keuthen NJ, Lochner C, Woods DW. Is trichotillomania a stereotypic movement disorder? An analysis of body-focused repetitive behaviors in people with hair-pulling. Ann Clin Psychiatry. 2008. PMID: 19034750
- Grant JE, Redden SA, Leppink EW, Chamberlain SR. Trichotillomania and co-occurring anxiety. Compr Psychiatry. 2017. PMID: 27668531
- Bloch MH, Landeros-Weisenberger A, Dombrowski P, Kelmendi B, Wegner R, Nudel J et al.. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry. 2007. PMID: 17727824
- Lee EB, Homan KJ, Morrison KL, Ong CW, Levin ME, Twohig MP. Acceptance and Commitment Therapy for Trichotillomania: A Randomized Controlled Trial of Adults and Adolescents. Behav Modif. 2020. PMID: 30117327