Introduction
Hair loss affects millions of women worldwide, creating significant emotional distress that extends far beyond physical appearance. While losing 50-100 hairs daily is completely normal, excessive hair loss can signal underlying medical conditions that require proper diagnosis and treatment. Understanding when hair shedding becomes concerning—and knowing which medical causes to investigate—empowers women to take control of their hair health and seek appropriate care.
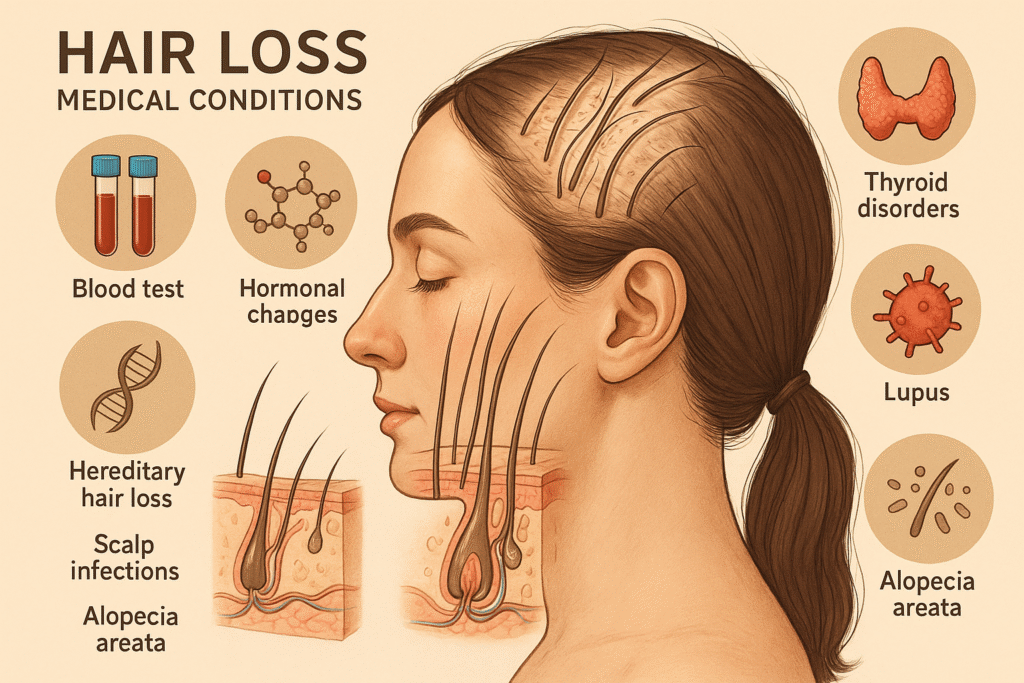
Unlike male pattern baldness, female pattern hair loss presents differently and often has multiple contributing factors. From hormonal imbalances to autoimmune conditions, the medical causes behind women’s hair loss are diverse and frequently treatable when identified correctly. The key lies in recognising the warning signs early and pursuing the right diagnostic approach.
This comprehensive guide examines the seven most common medical conditions responsible for hair loss in women. We’ll explore how genetic factors and hormonal changes contribute to thinning hair, investigate the role of thyroid disorders and nutritional deficiencies, and discuss autoimmune conditions that can cause sudden hair loss. You’ll also learn about stress-related shedding and how life transitions like pregnancy and menopause affect hair growth.
Beyond identifying causes, we’ll detail the essential diagnostic tests every woman should know about—from specific blood panels to specialised examinations that help pinpoint the root cause of hair loss. Most importantly, you’ll discover clear guidelines for when to seek professional help, ensuring you get the treatment you need to restore both your hair health and confidence.
Key Takeaways – TL/DR
- Seven major medical conditions commonly cause hair loss in women, including thyroid disorders and hormonal imbalances
- Specific blood tests and diagnostic procedures can identify the root cause of hair loss
- Early diagnosis and treatment can prevent permanent hair loss in many cases
- Female pattern baldness affects up to 40% of women by age 50
- Combining medical evaluation with appropriate testing leads to better treatment outcomes
Understanding Hair Loss in Women
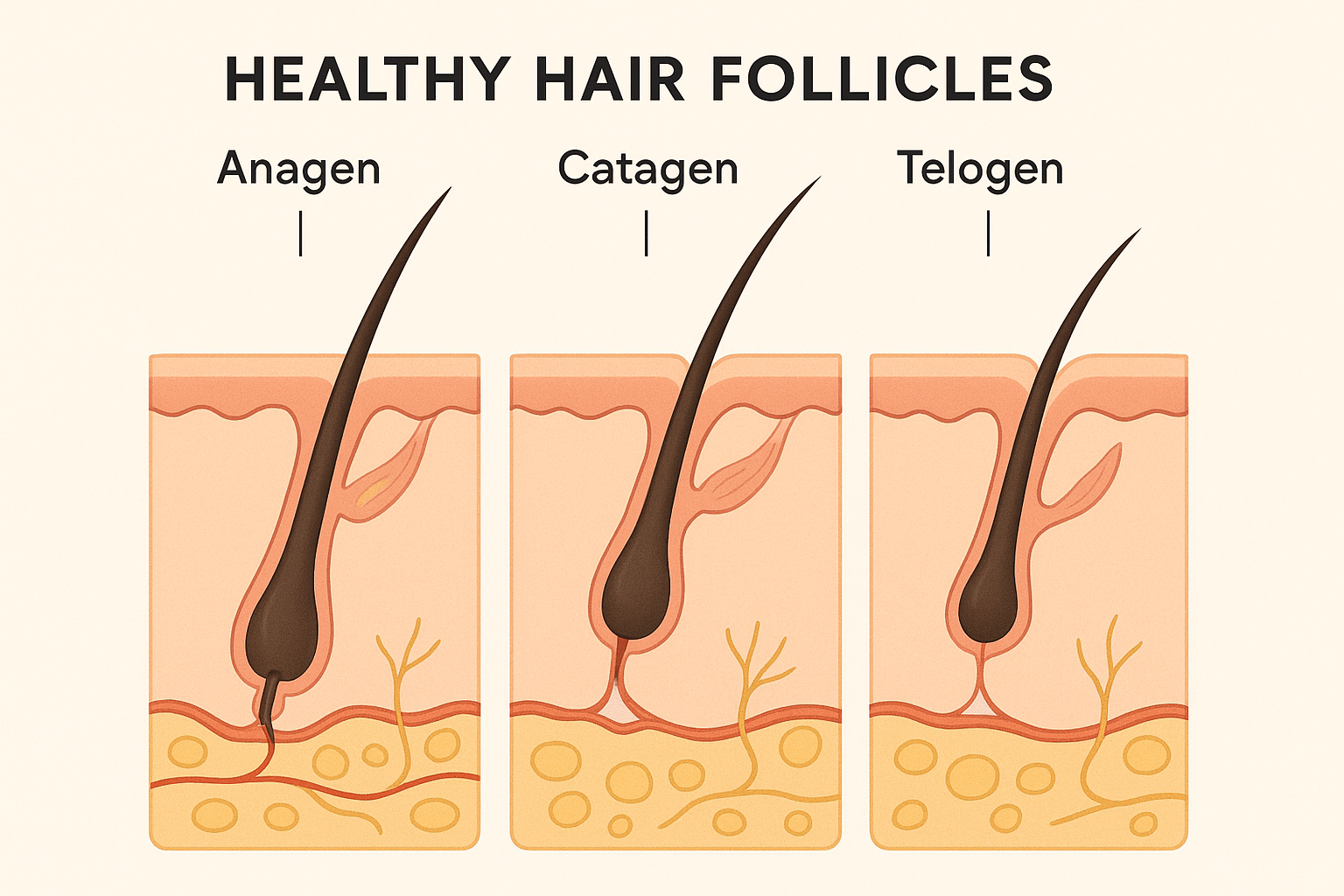
Understanding normal hair growth is essential for recognising when hair loss becomes problematic. Healthy hair follicles cycle through three distinct phases: anagen (growth), catagen (transition), and telogen (resting). During this natural process, losing 50-100 hairs daily is completely normal [1], as old hairs shed to make room for new growth. This continuous cycle maintains healthy hair density throughout life.
Hair loss becomes concerning when shedding exceeds 150 hairs per day or when noticeable hair thinning occurs. Women typically experience diffuse hair loss across the entire scalp rather than specific pattern baldness, making early detection challenging. Telogen effluvium, a common condition where hair follicles prematurely enter the resting phase, can cause sudden, widespread shedding following stress, illness, or hormonal changes.
Female hair loss patterns differ significantly from male presentations, often manifesting as gradual thinning along the part line or crown area while maintaining the frontal hairline. Understanding these distinctions helps women recognise when professional evaluation is necessary to maintain healthy hair and address underlying causes effectively.
Androgenetic Alopecia (Female Pattern Baldness)
Androgenetic alopecia, commonly known as female pattern baldness, represents the most prevalent cause of hair loss in women, affecting approximately 50% of women over age 50 [2]. This hereditary hair loss condition results from a complex interplay of genetic predisposition and hormonal influences, particularly involving androgen sensitivity that leads to progressive hair follicle miniaturization.
Genetic and Hormonal Factors
Female pattern baldness stems from inherited genetic variations that increase hair follicle sensitivity to dihydrotestosterone (DHT), a potent androgen derived from testosterone. Unlike simple dominant or recessive inheritance, androgenic alopecia follows a polygenic pattern, meaning multiple genes contribute to an individual’s susceptibility [3]. DHT binding to androgen receptors in genetically susceptible hair follicles triggers a gradual miniaturization process, causing follicles to produce progressively thinner, shorter hairs before eventually ceasing hair production entirely. This hereditary hair loss typically manifests when hormonal changes occur, such as during menopause when estrogen levels decline.
Progression Patterns in Women
Female pattern hair loss differs significantly from male baldness patterns, primarily affecting the crown and top of the scalp while preserving the frontal hairline. Women typically experience gradual hair density reduction, with widening of the central part being among the earliest visible signs. The Ludwig classification system describes three stages of progression, beginning with subtle thinning and advancing to more noticeable crown baldness while maintaining some hair coverage.

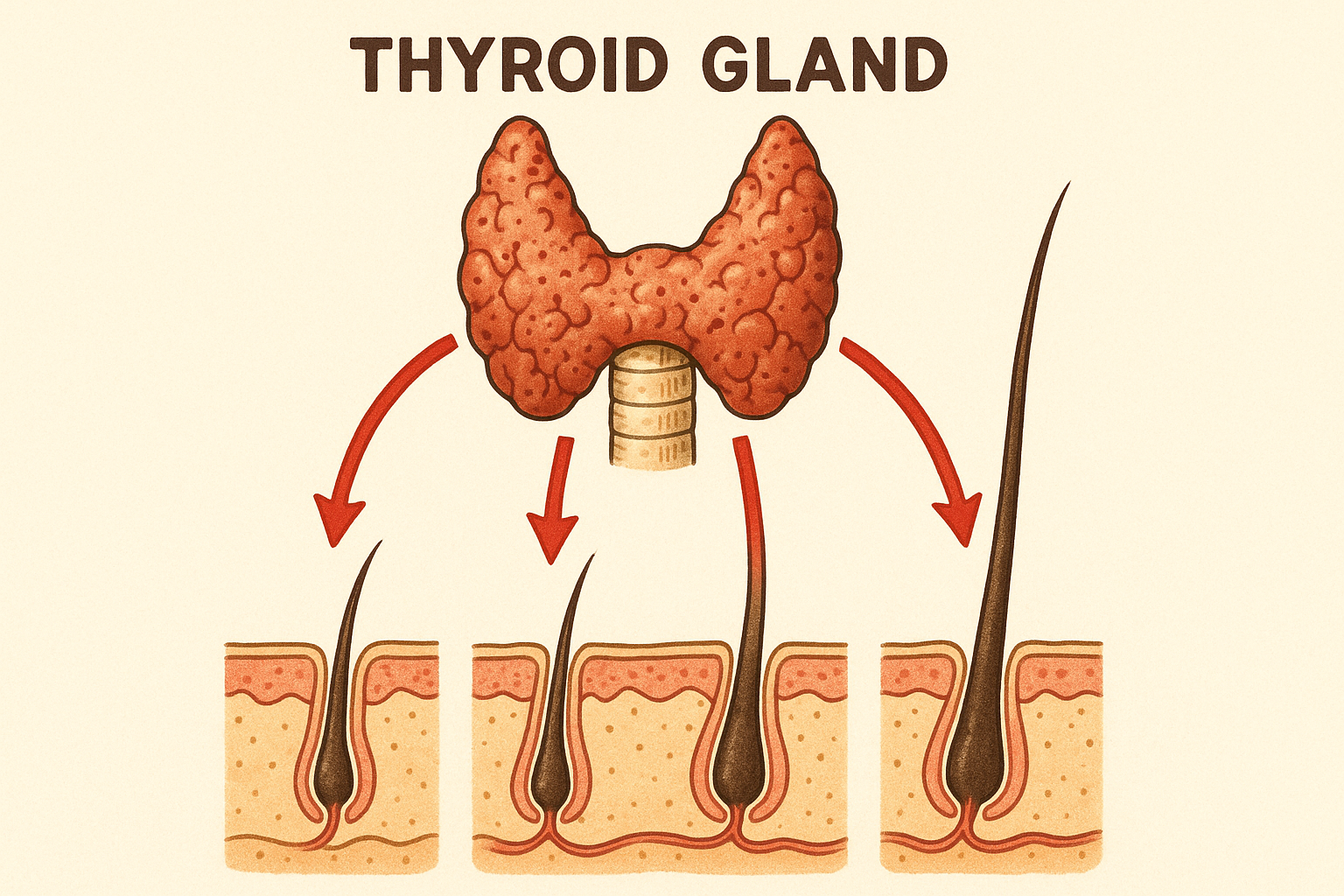
Thyroid Disorders and Hair Loss
Thyroid disease significantly impacts hair growth cycles, with both overactive and underactive thyroid conditions causing distinct patterns of hair loss. Women are disproportionately affected by thyroid disorders, with prevalence rates significantly higher than in men [4]. Fortunately, hair loss caused by thyroid dysfunction is typically temporary hair loss that responds well to proper thyroid management.
Hypothyroidism and Hair Thinning
An underactive thyroid slows metabolic processes, including hair growth cycles. This condition causes hair follicles to remain in the resting phase longer, resulting in diffuse thinning across the entire scalp. Hair texture becomes noticeably brittle and coarse, breaking easily during routine styling. The thinning pattern is typically uniform rather than concentrated in specific areas, distinguishing it from other types of hair loss. Once thyroid hormone levels normalise, patients can regrow hair as follicles resume normal cycling.
Hyperthyroidism Effects
Overactive thyroid accelerates hair growth cycles, paradoxically leading to increased shedding and fine, fragile hair texture. The rapid cycling exhausts hair follicles, causing accelerated hair loss throughout the scalp. Hair may appear thinner and feel silky or unusually soft. Like hypothyroid-related hair loss, this condition offers excellent potential for hair regrowth once thyroid function stabilises [5].
Iron Deficiency Anaemia
Iron deficiency creates a direct pathway to hair loss caused by insufficient nutrients reaching hair follicles. Women face particularly high vulnerability to this condition, with studies showing iron deficiency affects approximately 25% of women of reproductive age [6]. Proper blood tests can identify this treatable cause before significant hair loss occurs.
Why Women Are at Higher Risk
Women experience multiple factors that deplete iron stores and contribute to hair loss caused by nutritional deficiency. Monthly menstrual blood loss removes significant iron from the body, creating ongoing depletion that affects hair growth cycles. Pregnancy dramatically increases iron demands to support fetal development, often leaving maternal stores depleted. Additionally, many women struggle with dietary iron absorption due to factors like vegetarian diets or gastrointestinal conditions that impair nutrient uptake.
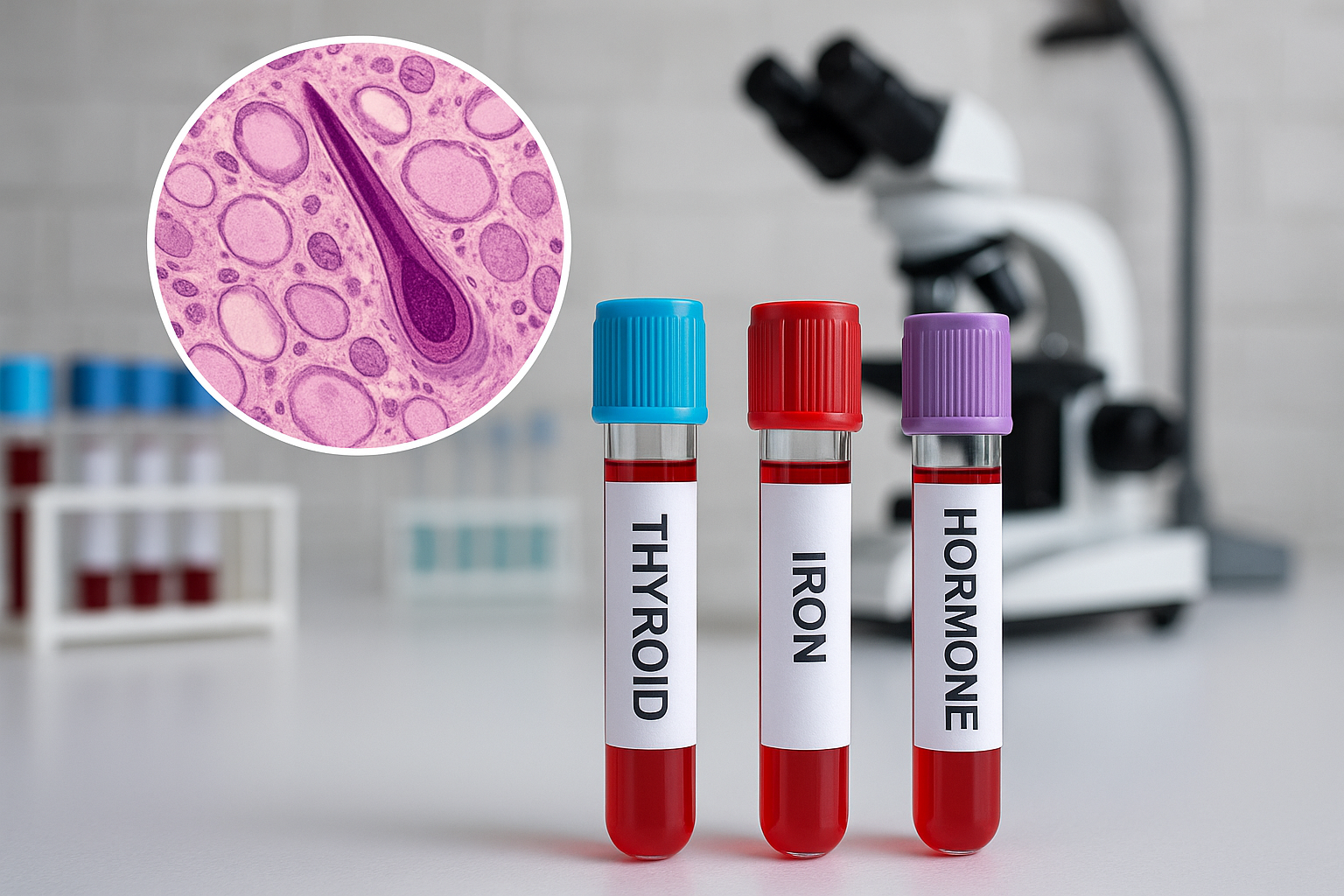
When treating hair loss linked to iron deficiency, comprehensive blood tests measuring ferritin levels are essential for accurate diagnosis. Addressing underlying iron deficiency can help stop hair loss progression and maintain healthy hair growth. Early detection through proper testing allows women to take targeted action before hair thinning becomes severe.
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) affects approximately 5-10% of reproductive-age women and commonly disrupts hair health through complex hormonal imbalances [7]. This endocrine disorder can simultaneously cause hair loss on the scalp while promoting unwanted hair growth elsewhere on the body.
Hormonal Imbalances in PCOS
Women with PCOS typically experience elevated androgen levels, particularly testosterone, which creates a cascade of hair-related effects . These elevated hormones increase sensitivity to dihydrotestosterone (DHT), the primary culprit behind androgenic alopecia. DHT miniaturises hair follicles on the scalp, leading to progressive thinning and hair loss caused by shortened growth cycles. Simultaneously, insulin resistance—common in PCOS—exacerbates androgen production and amplifies these effects. The paradoxical nature of PCOS-related hair changes becomes evident as the same hormonal imbalances that cause hair loss on the crown and temples often stimulate unwanted hair growth on the face, chest, and back. This dual pattern reflects varying follicle sensitivity across different body regions, highlighting how PCOS fundamentally disrupts normal hair health through systemic hormonal dysregulation.
Alopecia Areata
Alopecia areata is an autoimmune condition that causes distinctive patchy hair loss across the scalp and other body areas. This type of alopecia occurs when the immune system mistakenly targets healthy hair follicles, resulting in characteristic bald patches that can appear suddenly. Unlike other forms of hair loss, alopecia areata often allows hair to regrow spontaneously, though the condition can be unpredictable in its progression.
Autoimmune Attack on Follicles
The underlying mechanism of alopecia areata involves immune system dysfunction, where white blood cells incorrectly identify hair follicles as foreign threats. This misguided immune response triggers inflammation around the follicles, disrupting normal hair production cycles and causing existing hairs to fall out in distinct circular or oval bald patches. Fortunately, this autoimmune attack represents a reversible process, as the follicles themselves remain intact despite the inflammatory assault. The preserved follicle structure means individuals with this condition can regrow hair completely, often without medical intervention, though recurrence remains possible throughout a person’s lifetime.

Telogen Effluvium
Telogen effluvium represents one of the most common forms of temporary hair loss affecting women worldwide. This condition occurs when physical or emotional stress forces hair follicles to prematurely enter their resting phase, resulting in widespread hair thinning and excessive hair loss approximately two to three months after the triggering event.
Common Triggers
Several factors can trigger telogen effluvium in women. Major surgery places significant physical stress on the body, disrupting normal hair growth cycles and leading to noticeable hair loss weeks later. Severe illness, including high fevers, infections, or chronic conditions, similarly affects follicle function. Emotional stress from life changes, trauma, or prolonged anxiety can also precipitate this condition. Rapid weight loss, whether from dieting or medical conditions, deprives hair follicles of essential nutrients needed for healthy growth. Fortunately, telogen effluvium is reversible, and hair regrowth typically occurs once the underlying trigger resolves and stress levels normalize.
Hormonal Changes and Menopause
Natural hormonal changes throughout a woman’s life significantly impact hair health and can trigger various forms of hair loss. These fluctuations affect hair growth cycles, leading to temporary hair thinning or more permanent changes that resemble female pattern baldness.
Pregnancy and Postpartum Hair Loss
During pregnancy, elevated oestrogen levels extend the hair growth phase, creating thicker, fuller hair that many women enjoy. However, this hormonal advantage is temporary. After delivery, oestrogen levels drop dramatically, causing hair follicles to enter the resting phase simultaneously. This results in significant postpartum shedding, typically beginning 2-4 months after birth. Women may lose 300-500 hairs daily during this period, compared to the normal 50-100 strands. The good news is that postpartum hair loss represents a natural reset of hair growth cycles rather than permanent damage. Most women see their hair health return to pre-pregnancy levels within 6-12 months as hormonal changes stabilise and normal growth patterns resume.
Essential Diagnostic Tests to Request
Accurate diagnosis of hair loss requires systematic evaluation through comprehensive testing protocols that identify underlying medical conditions. Proper diagnostic workup combines blood tests, physical assessments, and specialised procedures to determine the specific cause affecting hair health and guide appropriate treatment strategies.
Blood Work Panel
Comprehensive blood tests form the foundation of hair loss evaluation, assessing hormonal imbalances and nutritional deficiencies. A complete blood count screens for anaemia and systemic conditions, while thyroid function panels including TSH, T3, and T4 detect thyroid disease that commonly triggers hair thinning . Iron studies measuring ferritin, serum iron, and total iron-binding capacity identify iron deficiency, a frequent culprit in female hair loss. Hormone level assessments should include testosterone, DHEA-S, and prolactin, with normal ranges varying by laboratory but typically testosterone levels below 70 ng/dL in women [8].
Physical Examination Tests
Physical examination begins with the pull test, where gentle traction on 50-100 hairs determines active shedding patterns. Scalp examination evaluates inflammation, scaling, or scarring that indicates specific hair loss conditions. Hair shaft examination under magnification reveals structural abnormalities, while assessment of hair distribution patterns helps differentiate between androgenetic alopecia and other causes.
Specialised Diagnostic Procedures
Advanced cases may require scalp biopsy when physical examination and blood tests remain inconclusive. Dermoscopy and trichoscopy provide detailed visualization of hair follicles and scalp conditions, offering non-invasive diagnostic insights that guide treatment decisions without surgical intervention.
When to See a Doctor
Seeking professional medical evaluation becomes essential when experiencing excessive hair loss that goes beyond normal daily shedding. If you notice sudden onset of patchy baldness, hair loss accompanied by scalp irritation, redness, or scaling, or if you’re losing more than 100 hairs daily for several weeks, it’s time to consult a Doctor. Early intervention can help prevent permanent hair loss and identify underlying medical conditions that may be contributing to the problem. Additionally, if hair loss significantly impacts your emotional well-being or if you have a family history of autoimmune disorders, professional evaluation can provide valuable insights into your hair health and appropriate treatment options.
Conclusion
Understanding the underlying medical conditions that contribute to hair loss represents a crucial first step in protecting your hair health and pursuing effective solutions. When women recognise the warning signs and seek proper medical evaluation, they position themselves to prevent permanent hair loss through targeted interventions.
The relationship between various medical conditions and hair loss demonstrates why comprehensive diagnostic testing with qualified healthcare providers remains essential. Whether dealing with thyroid disorders, hormonal imbalances, nutritional deficiencies, or autoimmune conditions, identifying the root cause enables personalised hair loss treatment approaches that address the source rather than just symptoms.
Early intervention consistently produces the best outcomes for women experiencing hair loss. Many underlying medical conditions respond well to treatment when detected promptly, allowing hair follicles to recover and resume normal growth cycles. Waiting too long often leads to more extensive damage that becomes increasingly difficult to reverse.
Taking proactive steps to evaluate your hair health through medical assessment empowers you to make informed decisions about treatment options. Remember that numerous causes of hair loss are completely reversible when appropriate medical care is sought early. Working collaboratively with healthcare professionals ensures you receive evidence-based treatments tailored to your specific medical profile and hair loss pattern.
Frequently Asked Questions
Women typically lose 50-100 hairs per day as part of the natural hair growth cycle. Losing more than 150 hairs daily for several weeks may indicate a medical condition requiring evaluation.
Stress typically causes temporary hair loss called telogen effluvium. However, chronic stress can worsen genetic hair loss patterns and potentially lead to more permanent thinning if left untreated.
While blood tests can identify current medical causes of hair loss, they cannot predict future genetic hair loss.
Hair regrowth typically begins 3-6 months after addressing the underlying medical cause, as hair follicles need time to reset their growth cycle. Full recovery may take 12-18 months.
References
- Malkud S. A Hospital-based Study to Determine Causes of Diffuse Hair Loss in Women. J Clin Diagn Res. 2015. PMID: 26436027
- Blume-Peytavi U, Blumeyer A, Tosti A, Finner A, Marmol V, Trakatelli M et al.. S1 guideline for diagnostic evaluation in androgenetic alopecia in men, women and adolescents. Br J Dermatol. 2011. PMID: 20795997
- Heilmann S, Brockschmidt FF, Hillmer AM, Hanneken S, Eigelshoven S, Ludwig KU et al.. Evidence for a polygenic contribution to androgenetic alopecia. Br J Dermatol. 2013. PMID: 23701444
- Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012. PMID: 22273398
- Kantor J, Kessler LJ, Brooks DG, Cotsarelis G. Decreased serum ferritin is associated with alopecia in women. J Invest Dermatol. 2003. PMID: 14708596
- Camaschella C. Iron deficiency. Blood. 2019. PMID: 30401704
- Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018. PMID: 29569621
- Rossi A, Cantisani C, Melis L, Iorio A, Scali E, Calvieri S. Minoxidil use in dermatology, side effects and recent patents. Recent Pat Inflamm Allergy Drug Discov. 2012. PMID: 22409453