Introduction
Hair loss during menopause affects millions of women worldwide, yet the experience varies significantly depending on whether menopause occurs naturally or surgically. Understanding these differences is crucial for managing expectations and seeking appropriate treatment for hair thinning concerns.
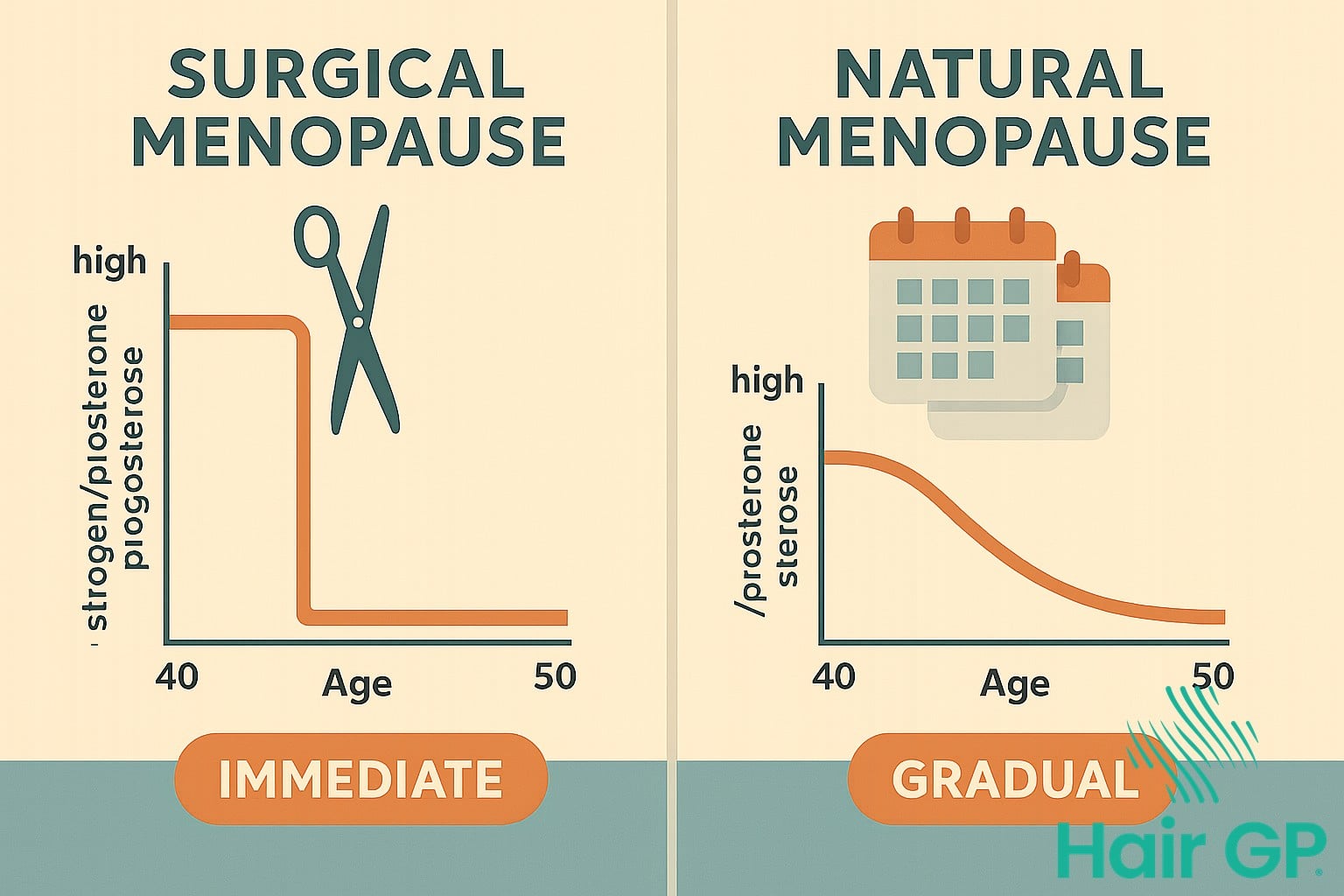
Natural menopause typically unfolds gradually over several years, allowing the body to adjust slowly to declining hormone levels. In contrast, surgical menopause—resulting from removal of both ovaries—triggers an immediate and dramatic drop in oestrogen and progesterone, leading to more abrupt hormonal changes.
These distinct pathways to menopause create different patterns of hair loss. Women experiencing natural menopause often notice gradual thinning over time, whilst those undergoing surgical menopause may face more sudden and pronounced changes to their hair density and texture.
This comprehensive guide explores how each type of menopause affects the hair growth cycle, examining the specific patterns of hair loss associated with both natural and surgical transitions. We’ll compare onset timing, severity, and recovery potential, whilst providing evidence-based treatment options tailored to your specific situation. Additionally, we’ll help you identify risk factors and understand when professional guidance becomes essential for maintaining optimal hair health during this significant life transition.
Key Takeaways – TL/DR
- Surgical menopause causes more sudden and severe hair loss due to abrupt hormonal changes
- Natural menopause leads to gradual hair thinning over months or years
- Both types can be treated with hormone therapy, topical minoxidil, and lifestyle changes
- Hair loss patterns differ in timing, severity, and reversibility between the two types
- Early intervention improves treatment outcomes for both menopause-related hair loss types
Understanding Surgical vs Natural Menopause
Understanding the distinction between surgical and natural menopause helps women navigate their unique hormonal transitions more effectively. Whilst natural menopause develops gradually over years, surgical menopause creates an immediate cessation of hormone production, leading to vastly different experiences and management approaches.
What Triggers Surgical Menopause
Surgical menopause occurs when medical interventions abruptly halt ovarian function, instantly stopping hormone production. The most common cause is bilateral oophorectomy—removal of both ovaries—which immediately eliminates the body’s primary source of oestrogen and progesterone. This procedure may accompany a complete hysterectomy for various medical reasons, including cancer prevention or treatment. Cancer treatments, particularly pelvic radiation and certain chemotherapy regimens, can also damage ovarian tissue irreversibly, triggering premature menopause.[1]
Unlike natural menopause, where hormones decline gradually, surgical menopause creates an immediate hormonal void. Women experience this dramatic shift overnight, with no adjustment period for their bodies to adapt. Approximately 12-15% of women undergo surgical menopause before reaching natural menopause age.[2]
Natural Menopause Timeline
Natural menopause represents a gradual biological transition occurring around age 51 in most women.[3] This process begins with perimenopause, a phase lasting 4-8 years where hormone fluctuations create irregular periods and various symptoms.[4] During perimenopause, oestrogen and progesterone levels rise and fall unpredictably, causing the characteristic hot flushes, mood changes, and menstrual irregularities.
The transition progresses through distinct stages: early perimenopause with subtle cycle changes, late perimenopause with increased symptoms and longer gaps between periods, and finally, complete cessation of menstruation for twelve consecutive months, marking official menopause. This extended timeline allows women’s bodies to adjust gradually to declining hormone levels, often resulting in milder symptoms compared to the abrupt changes of surgical menopause.
How Hormones Affect Hair Growth Cycle
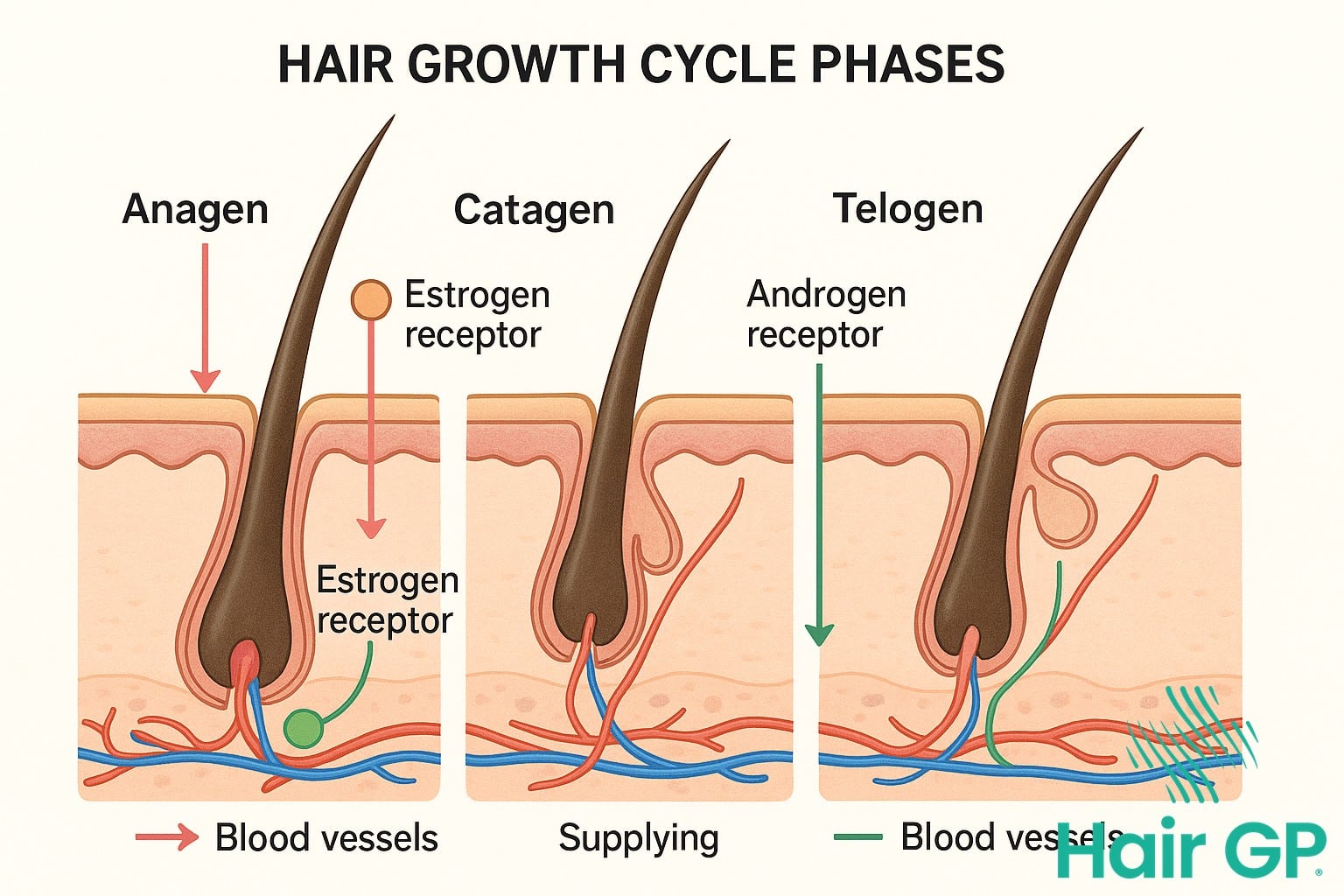
The intricate relationship between hormones and the hair growth cycle becomes particularly evident during menopause, when shifting hormone levels can dramatically affect hair health. Understanding how oestrogen, progesterone, and androgens influence human hair follicles helps explain why many women experience significant hair changes during this transition.
The normal hair growth cycle consists of three phases: anagen (growth), catagen (transition), and telogen (resting). In healthy adults, approximately 85-90% of scalp hair follicles remain in the active growth phase[5], which typically lasts between two to seven years. Hormonal fluctuations during menopause can disrupt this delicate balance, leading to shortened growth phases and prolonged resting periods.
The Role of Oestrogen in Hair Health
Oestrogen plays a crucial protective role in maintaining healthy hair growth by extending the anagen phase and increasing hair diameter. This hormone helps maintain the hair follicle’s metabolic activity and promotes the production of growth factors that support robust hair development. Additionally, oestrogen acts as a natural shield against androgens, preventing these male sex hormones from binding to receptors within the hair follicle.
When oestrogen levels decline during menopause, hair follicles lose this protective influence. The result is often thinner, more fragile hair strands that spend less time in the active growth phase, leading to overall hair thinning and reduced density.
Androgen Effects on Hair Follicles
As oestrogen levels drop, the relative influence of androgens increases, even though their absolute levels may remain unchanged. Dihydrotestosterone (DHT), the most potent androgen, plays a significant role in female pattern hair loss, affecting up to 40% of women by age 50[6]. DHT binds to receptors in susceptible hair follicles, triggering a process called miniaturisation.
This miniaturisation process causes the hair follicle to progressively shrink with each growth cycle, producing increasingly finer and shorter hairs. The pattern of DHT-related hair loss typically affects the crown and frontal scalp areas, whilst sparing the occipital region where follicles show less sensitivity to androgens. Understanding these hormonal mechanisms helps explain why menopausal hair loss follows specific patterns and why targeted treatments focusing on hormone balance often prove most effective.
Hair Loss Patterns in Natural Menopause
During natural menopause, women experience distinctive hair thinning patterns that develop gradually as oestrogen levels decline. Unlike sudden hair loss conditions, menopausal changes follow predictable patterns across the scalp, helping women recognise and understand these transformations. The progression typically spans several years, with specific areas showing more vulnerability to hormonal fluctuations.
Common Thinning Locations
The crown area typically reveals the first signs of menopausal hair thinning, where women notice increased scalp visibility through their hair. This central thinning often accompanies a gradually widening part, which becomes more pronounced as follicles produce finer, weaker strands. Many women observe their once-narrow parting expanding into a broader line, particularly noticeable when styling or photographing from above.
Temple recession represents another characteristic pattern, though less dramatic than male-pattern baldness. The hairline may subtly retreat at the temples, creating a slightly altered facial frame. Some women experience diffuse thinning across the entire scalp rather than localised loss, resulting in overall reduced volume without distinct bald patches. This generalised pattern can make ponytails feel thinner and reduce the hair’s ability to hold styles effectively.
Timeline and Progression
Hair changes often begin during perimenopause onset, typically starting 2-8 years before final menstruation[1]. Initial changes manifest subtly—increased shedding during washing, more hair accumulating in brushes, or slight volume reduction. These gradual changes distinguish menopausal patterns from acute telogen effluvium, where temporary hair loss occurs rapidly following specific triggers.
The progression intensifies as oestrogen continues declining, with most women noticing definitive thinning within 12-24 months of their final period[2]. However, this isn’t always permanent; many experience a stabilisation period approximately 2-3 years post-menopause when shedding rates normalise. During this phase, whilst hair may remain thinner than pre-menopausal density, active loss typically ceases.
Understanding these patterns helps differentiate normal menopausal changes from other conditions requiring medical attention. Recognising the gradual nature prevents unnecessary anxiety whilst encouraging timely intervention when patterns deviate from expected progression.

Hair Loss Patterns in Surgical Menopause
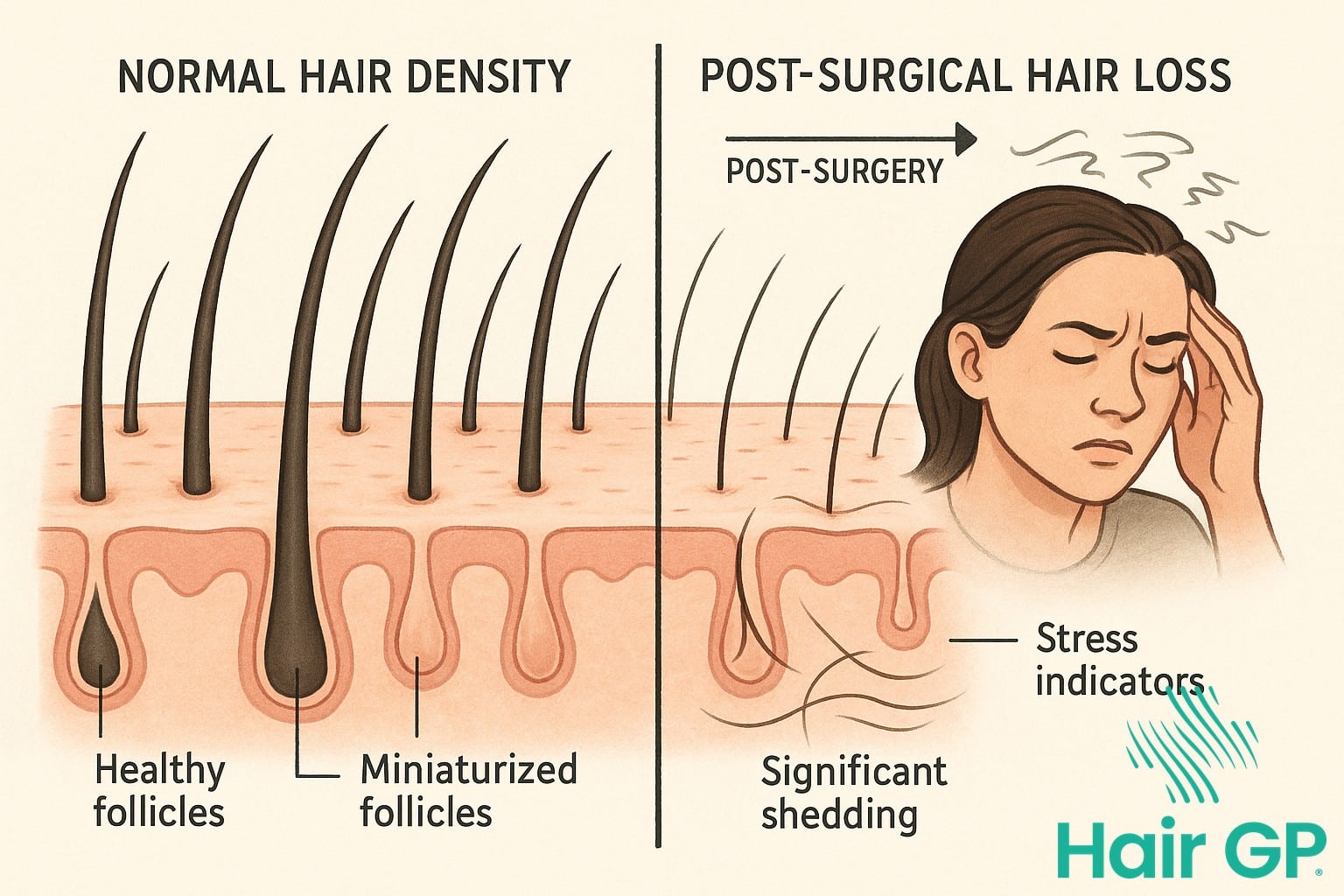
Surgical menopause triggers distinctly different hair loss patterns compared to natural menopause, with more rapid onset and potentially severe manifestations. The abrupt cessation of ovarian hormones following bilateral oophorectomy creates an immediate hormonal shock that profoundly impacts hair follicle cycling, often resulting in dramatic shedding within weeks of surgery.
Immediate Post-Surgical Changes
The sudden hormonal withdrawal following surgical menopause frequently precipitates telogen effluvium, a stress-induced form of temporary hair loss characterised by widespread shedding. Studies indicate that up to 70% of women experience significant hair loss within three months post-surgery[7]. This acute phase typically begins 6-12 weeks after the procedure, as follicles prematurely shift from the growth phase into the resting phase.
Multiple stress factors compound the hair loss experience during this period. The physical trauma of surgery itself initiates a systemic stress response that can independently trigger telogen effluvium. Additionally, the psychological stress of adapting to sudden menopause, combined with potential anaesthesia effects and nutritional disruptions during recovery, creates a perfect storm for follicular dysfunction. Unlike gradual menopausal transitions, this abrupt change offers no adaptation period for hair follicles to adjust to declining hormone levels.
Long-Term Pattern Development
As the initial shock subsides, many women develop androgenetic alopecia patterns characterised by central scalp thinning and widening of the part line. Without the protective effects of oestrogen, follicles become increasingly sensitive to androgens, leading to progressive miniaturisation. While some experience partial recovery within 6-12 months, research suggests that only 40-60% achieve complete hair density restoration[8].
The recovery potential varies significantly based on individual factors including age at surgery, genetic predisposition, and hormone replacement therapy initiation. Some women experience permanent changes in hair texture and density, with finer, more brittle strands replacing previously thick hair. Early intervention with appropriate treatments can improve outcomes, though the reversible nature of surgical menopause-induced hair loss depends heavily on addressing underlying medical conditions and hormonal imbalances promptly. Understanding these distinct patterns helps clinicians differentiate between temporary stress-related shedding and progressive androgenetic changes requiring different therapeutic approaches.
Comparing Onset, Severity, and Recovery
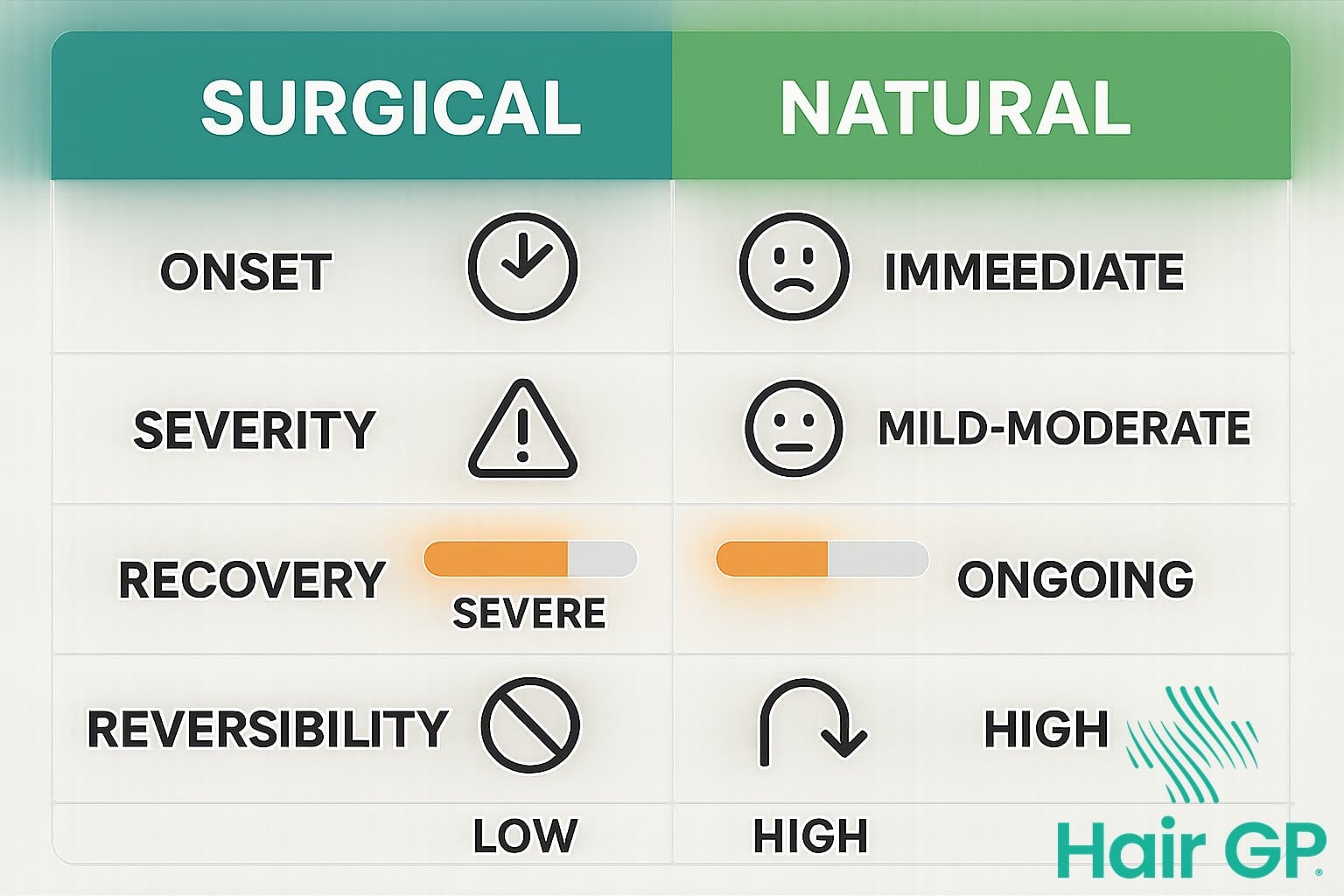
The timing of hair loss related changes differs markedly between surgical and natural menopause. Surgical menopause triggers an immediate hormonal shift, with hair changes often appearing within weeks or months post-surgery. In contrast, natural menopause involves a gradual transition over several years, allowing follicles to adapt more slowly to declining oestrogen levels. This extended period of hormonal adjustment typically results in less dramatic initial changes.
Severity patterns also vary significantly between the two types. Women experiencing surgical menopause often face more intense hair loss initially, as follicles struggle to cope with the sudden hormonal withdrawal. Natural menopause generally produces milder symptoms that progress gradually, though individual responses vary considerably. Neither type typically leads to complete baldness, unlike androgenetic alopecia in men, but surgical menopause may create more noticeable thinning in the short term.
Recovery potential and timelines present encouraging news for both groups. Hair loss from surgical menopause is often reversible, particularly when hormone replacement therapy begins promptly. Recovery may take longer for surgical cases, typically requiring 6-12 months for noticeable improvement. Natural menopause hair changes may stabilise more readily once hormones find their new balance, though regrowth depends on various factors including genetics, nutrition, and overall health. Early intervention improves outcomes for both types, with treatments proving most effective when started at the first signs of thinning rather than waiting for significant loss to occur.
Treatment Options for Menopause Hair Loss
Effective treatment for menopause-related hair loss requires a comprehensive approach tailored to individual needs and menopause type. Both medical interventions and lifestyle modifications can significantly improve hair density and prevent further loss, with treatment strategies varying based on whether women experience natural or surgical menopause.
Medical Treatments and Medications
Hormone replacement therapy (HRT) remains a cornerstone treatment for menopause-related hair loss, particularly effective in surgical menopause cases. Studies demonstrate that oestrogen therapy can improve hair density in up to 63% of postmenopausal women[9]. For localised treatment, topical minoxidil stands as the only FDA-approved medication for female pattern hair loss, with 2% and 5% formulations showing efficacy. Clinical trials indicate that 5% minoxidil produces superior results, with approximately 44% of women experiencing moderate hair growth after 24 weeks of treatment[10].
Anti-androgen medications, including spironolactone and finasteride, offer additional options for women experiencing androgen-related thinning. These hair loss medications work by blocking testosterone’s effects on hair follicles, though they require careful monitoring and are contraindicated during pregnancy. Some practitioners combine topical minoxidil with oral medications to maximise new hair growth potential, particularly in cases resistant to monotherapy.
Natural and Lifestyle Approaches
Nutritional support plays a vital role in maintaining healthy hair during menopause. Essential nutrients including iron, vitamin D, biotin, and omega-3 fatty acids support follicle health and hair growth cycles. Regular scalp massage increases blood circulation, potentially enhancing the effectiveness of topical treatments whilst promoting relaxation.
Stress reduction techniques prove particularly beneficial, as chronic stress exacerbates hormonal imbalances and hair loss. Mindfulness meditation, yoga, and regular exercise help regulate cortisol levels whilst improving overall wellbeing. Gentle hair care practices, including reduced heat styling and chemical processing, prevent additional damage to vulnerable hair.
Emerging hair loss treatments show promise, including platelet-rich plasma therapy and low-level laser therapy, though further research is needed to establish optimal protocols for menopausal women. Success often requires patience and consistency, with most treatments requiring three to six months before visible improvements occur.

Risk Factors and When to Seek Help
Certain risk factors significantly increase the likelihood of experiencing hair loss during both surgical and natural menopause. Women with pre-existing medical conditions such as thyroid disorders, iron deficiency anaemia, or autoimmune diseases face heightened vulnerability. Additionally, those undergoing chemotherapy or radiation therapy alongside surgical menopause often experience compounded hair loss effects. Nutritional deficiencies, chronic stress, and certain prescribed medications can further exacerbate hair thinning regardless of menopause type.
Recognising when to consult a doctor or specialist physician is crucial for proper management. Seek professional help if you notice sudden, patchy hair loss, scalp pain or inflammation, or if hair thinning is accompanied by other concerning symptoms like unexplained weight changes or extreme fatigue. Women experiencing severe side effects from hormone replacement therapy that affect hair health should also schedule an immediate consultation.
During your medical evaluation, expect a comprehensive assessment including blood tests to check hormone levels, nutritional status, and thyroid function. Your healthcare provider will review your medical history, current medications, and perform a scalp examination. This thorough approach ensures accurate diagnosis and appropriate treatment planning tailored to your specific situation.
Conclusion
Understanding the distinct hair loss patterns between surgical menopause and natural menopause proves crucial for selecting effective treatment options. Whilst natural menopause typically causes gradual thinning, surgical menopause often triggers rapid, widespread shedding requiring immediate intervention. These fundamental differences demand tailored approaches rather than one-size-fits-all solutions.
Recognising your specific type enables targeted treatments that address underlying causes rather than merely managing symptoms. Women experiencing surgical menopause may benefit from hormone replacement therapy discussions with their doctor, whilst those in natural menopause might find success with minoxidil or nutritional support for hair growth stimulation.
Proactive management remains essential regardless of menopause type. Early intervention typically yields better outcomes than delayed treatment. Consulting healthcare professionals who understand hormonal hair loss ensures comprehensive care addressing both immediate concerns and long-term follicular health. Remember, whilst menopausal hair loss presents challenges, informed decisions and appropriate treatments can significantly improve hair density and confidence.
Frequently Asked Questions
Hair loss typically begins 2-3 months after surgery due to telogen effluvium, with peak shedding occurring around 3-4 months. The sudden hormonal shock triggers a larger percentage of hair follicles to enter the resting phase simultaneously.
While complete reversal depends on various factors, many women see improvement with treatment. Surgical menopause hair loss often responds better to treatment if addressed early. Natural menopause hair loss may stabilize but rarely returns to pre-menopausal density without ongoing treatment.
Yes, topical minoxidil is generally safe for menopausal women and is FDA-approved for female pattern hair loss. Side effects are typically mild and may include scalp irritation. Always consult your doctor before starting treatment, especially if you have other medical conditions.
If you’re experiencing perimenopause symptoms or planning surgical menopause, preventive measures can be beneficial. These include optimizing nutrition, managing stress, and discussing hormone therapy options with your healthcare provider. Early intervention often yields better results.
References
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483-491.
- Rocca WA, Gazzuola Rocca L, Smith CY, et al. Bilateral Oophorectomy and Accelerated Aging: Cause or Effect? J Gerontol A Biol Sci Med Sci. 2017;72(9):1213-1217.
- Shifren JL, Gass ML; NAMS Recommendations for Clinical Care of Midlife Women Working Group. The North American Menopause Society recommendations for clinical care of midlife women. Menopause. 2014;21(10):1038-1062.
- Santoro N, Roeca C, Peters BA, Neal-Perry G. The Menopause Transition: Signs, Symptoms, and Management Options. J Clin Endocrinol Metab. 2021;106(1):1-15.
- Grymowicz M, Rudnicka E, Podfigurna A, et al. Hormonal Effects on Hair Follicles. Int J Mol Sci. 2020;21(15):5342.
- Ramos PM, Miot HA. Female Pattern Hair Loss: a clinical and pathophysiological review. An Bras Dermatol. 2015;90(4):529-543.
- Ramos PM, Miot HA. Female Pattern Hair Loss: a clinical and pathophysiological review. An Bras Dermatol. 2015;90(4):529-543.
- Starace M, Orlando G, Alessandrini A, Piraccini BM. Female Androgenetic Alopecia: An Update on Diagnosis and Management. Am J Clin Dermatol. 2020;21(1):69-84.
- Birch MP, Lalla SC, Messenger AG. Female pattern hair loss. Clin Exp Dermatol. 2002;27(5):383-388.
- Blume-Peytavi U, Hillmann K, Dietz E, et al. A randomized, single-blind trial of 5% minoxidil foam once daily versus 2% minoxidil solution twice daily in the treatment of androgenetic alopecia in women. J Am Acad Dermatol. 2011;65(6):1126-1134.