Introduction
When experiencing hair loss, many patients receive blood tests that return completely normal results—yet their hair continues to thin. This disconnect highlights a crucial truth about scalp level diagnosis: what blood work can’t tell about hair loss often holds the key to effective treatment. Whilst laboratory tests provide valuable insights into systemic health, they cannot reveal the complex processes occurring directly within hair follicles and the surrounding scalp tissue.
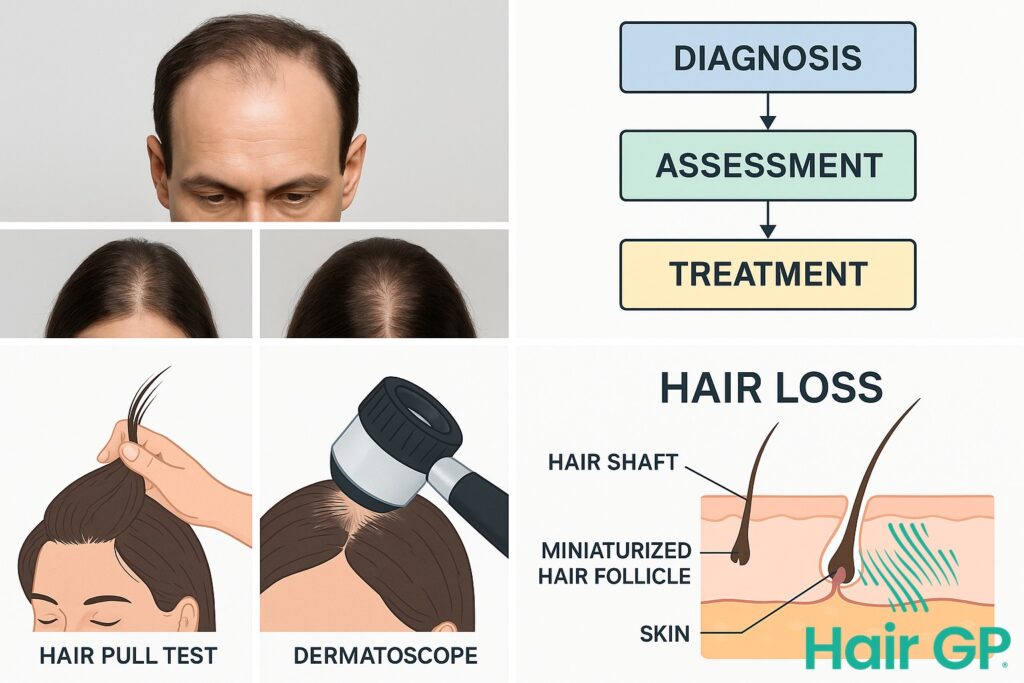
Understanding the underlying cause of hair loss requires comprehensive assessment beyond standard blood tests. Hair growth cycles, follicular miniaturisation patterns, and localised inflammatory processes all escape detection through laboratory analysis alone. Physical examination techniques including trichoscopy and dermoscopy reveal critical diagnostic information about follicular health, scarring patterns, and specific hair loss conditions that would otherwise remain unidentified.
This article explores the essential diagnostic tests that complement blood work in hair loss evaluation. We’ll examine how hair growth cycle disruptions manifest clinically, why conditions like female pattern baldness and alopecia areata require visual assessment for diagnosis, and when advanced techniques such as scalp biopsy become necessary. You’ll discover how integrating multiple diagnostic approaches creates a complete picture of hair loss causation, enabling targeted treatment strategies based on scalp-level findings rather than laboratory values alone.
Key Takeaways – TL/DR
- Normal blood test results don’t rule out treatable hair loss conditions like androgenetic alopecia or alopecia areata
- Scalp biopsy can identify inflammatory patterns invisible to blood work, revealing 85% more diagnostic information
- Trichoscopy and dermoscopy detect early miniaturization patterns 6-12 months before visible hair loss
- Physical examination techniques like the pull test provide immediate diagnostic value unavailable through laboratory testing
Understanding Hair Growth Cycles and Their Diagnostic Importance
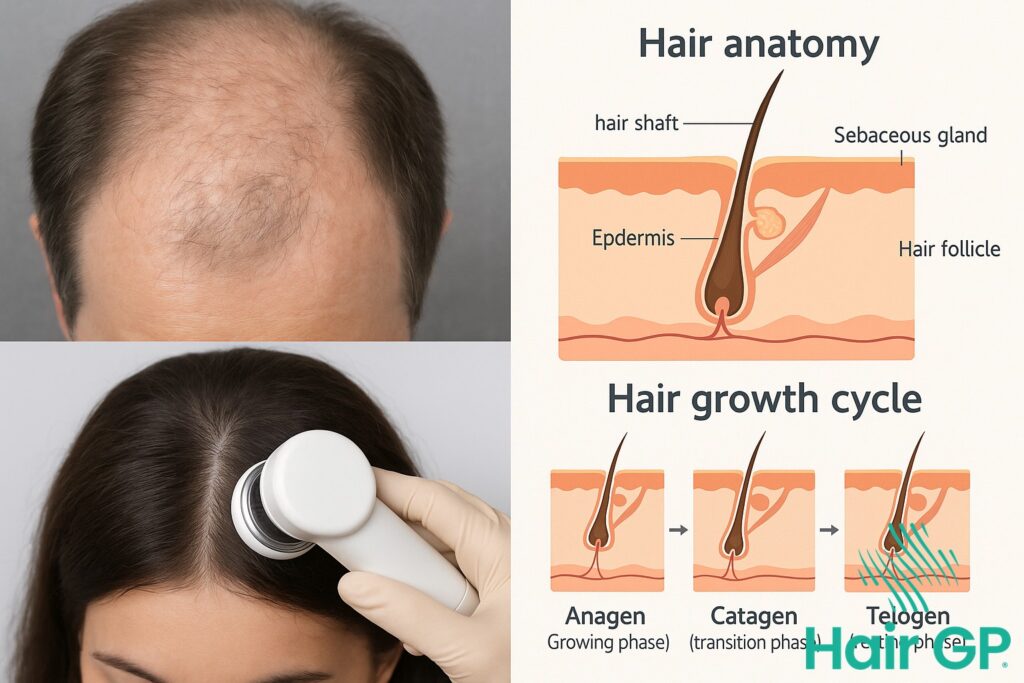
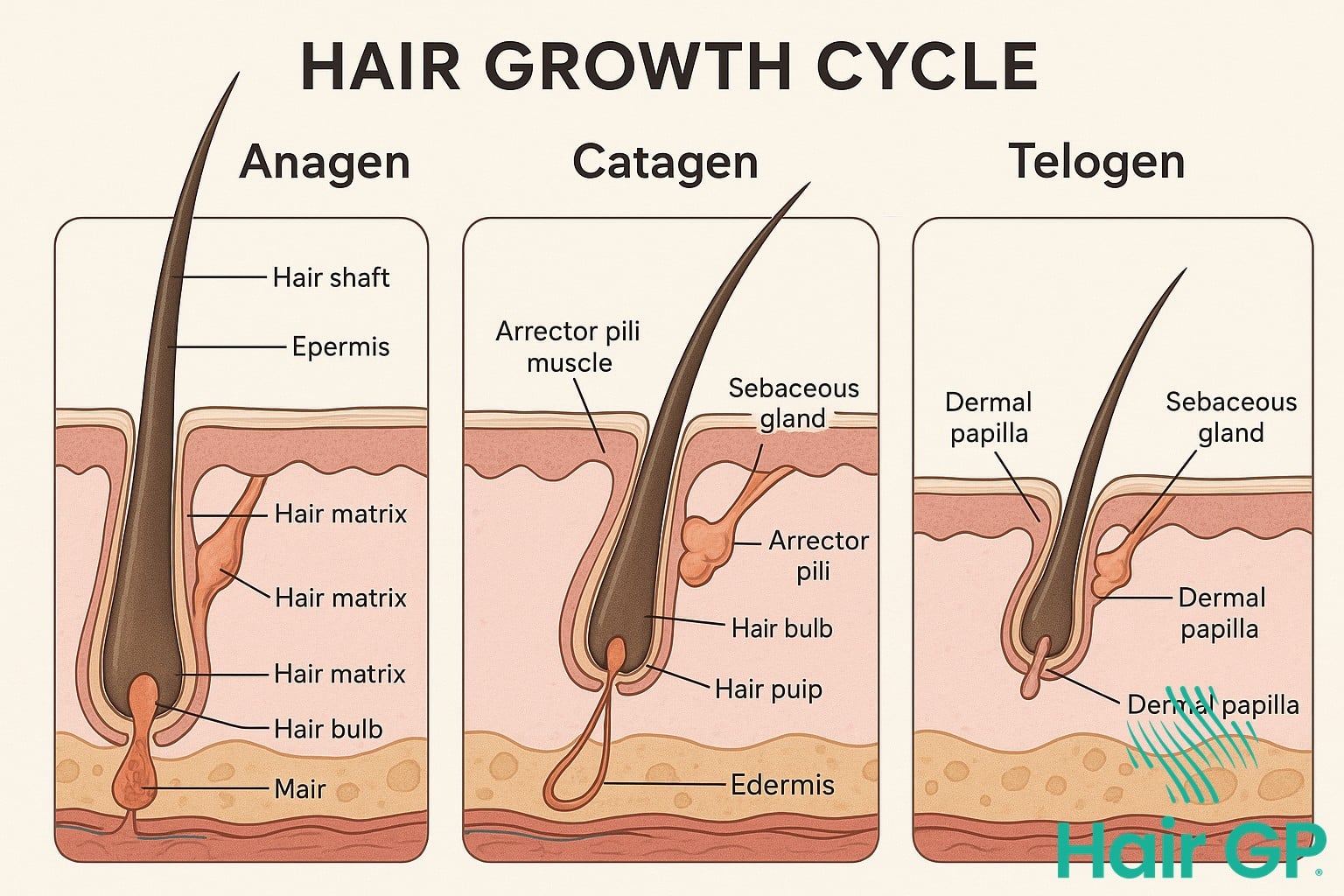
Hair follicles undergo continuous cycling through three distinct phases that directly affect hair growth and loss patterns. The anagen (growth) phase typically lasts 2-7 years, catagen (transition) 2-3 weeks, and telogen (resting phase) approximately 3 months, with 85-90% of scalp hairs normally in anagen at any time [1]. Understanding these phases proves essential for diagnosis, as disruptions invisible to blood work manifest through altered growth cycle timing and follicular miniaturisation.
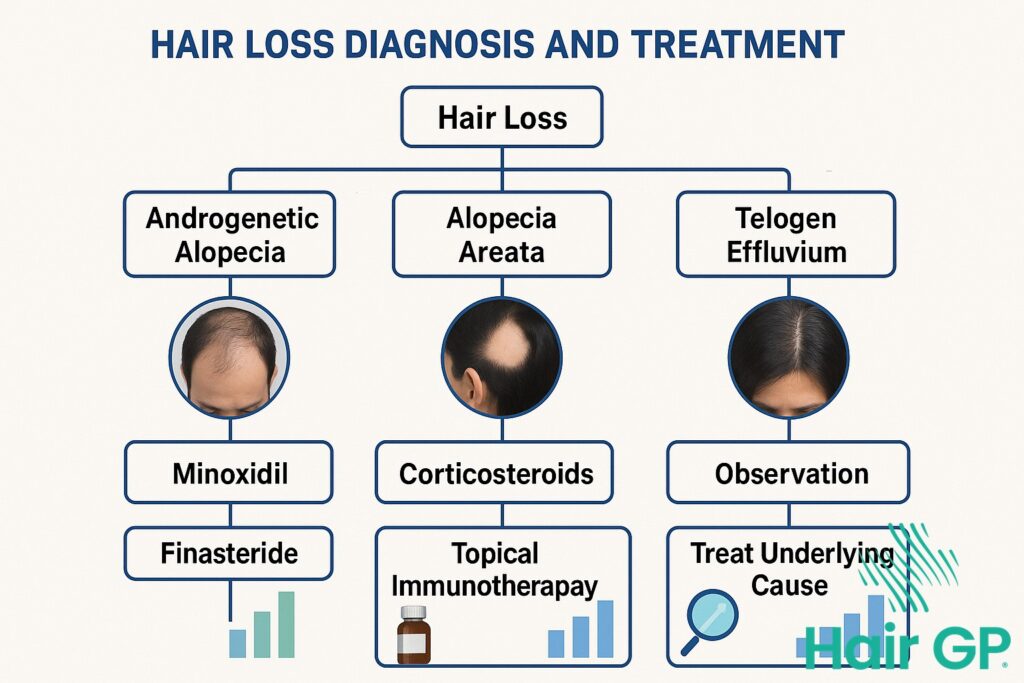
When the hair growth cycle becomes disrupted, conditions like telogen effluvium push excessive follicles into the resting phase prematurely, whilst androgenetic alopecia progressively shortens anagen duration [2]. These cycle abnormalities cannot be detected through laboratory tests but profoundly affect hair growth patterns. Blood markers remain normal even as follicles fail to complete proper cycles, preventing new hair growth and causing progressive thinning that may slow hair growth over time.
Detecting Shortened Anagen Phase Through Physical Examination
Dermoscopy reveals critical anagen phase abnormalities through direct visualisation of hair shafts and follicular units. Shortened anagen manifests as decreased shaft diameter variations, with increasing vellus hair percentage indicating cycle disruption. The terminal to vellus ratio provides quantifiable evidence of miniaturisation, whilst broken hairs and abundant short hairs suggest premature cycle termination. These physical findings guide treatments that stimulate hair growth and promote hair regrowth effectively.
Hair Follicles: What Physical Scalp Examination Reveals
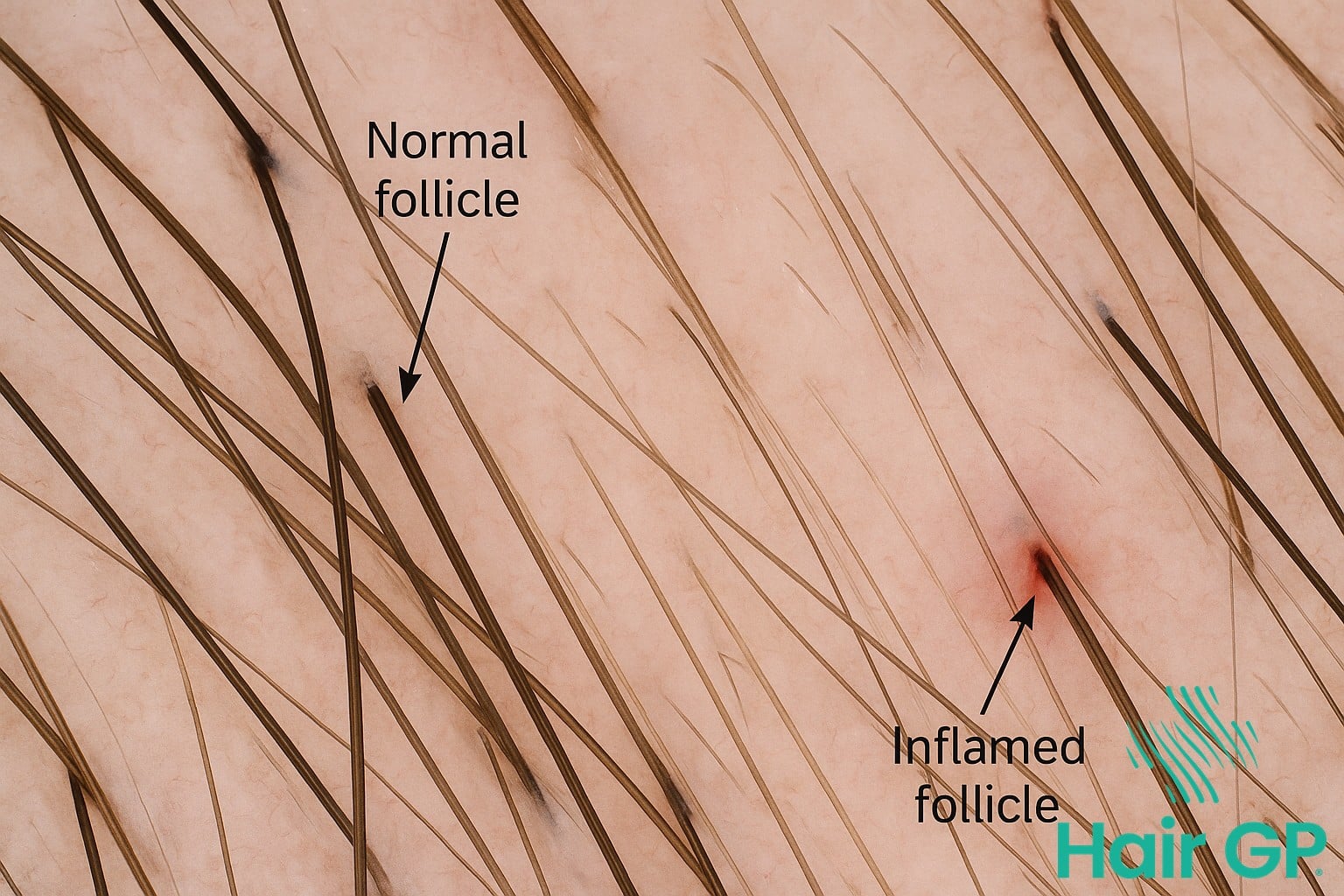
Direct examination of hair follicles reveals critical diagnostic information that blood tests cannot detect. Through trichoscopy and dermoscopy, clinicians can visualise follicular structures, inflammation patterns, and scarring processes occurring at the scalp level, achieving diagnostic accuracy rates of up to 96% for certain conditions[3]. Physical examination of scalp skin and follicular units provides immediate insights into miniaturization severity, perifollicular changes, and early signs of conditions like scarring alopecia or folliculitis.
Miniaturization Patterns in Androgenetic Alopecia
Follicular miniaturization represents the hallmark finding in androgenetic alopecia, with trichoscopy revealing progressive diameter reduction in affected follicular units[4]. During physical examination, clinicians assess the terminal-to-vellus hair ratio, with more than 20% miniaturized hairs indicating pattern baldness progression. Hair follicles undergo predictable transformation patterns: terminal hairs gradually thin from 60-80 micrometres to vellus-like structures under 30 micrometres in diameter. Trichoscopic analysis of hair roots and scalp and hair interfaces reveals diversity in follicular unit composition—normally containing 2-4 terminal hairs, these units progressively display single miniaturized follicles in advanced cases. This direct visualisation enables precise staging of male pattern baldness severity, something blood markers cannot quantify despite normal hormone levels.
Blood Tests: Essential Yet Limited in Hair Loss Diagnosis
Blood tests provide crucial baseline information in hair loss evaluation, yet their diagnostic scope remains inherently limited. Complete blood count assessments can identify iron deficiency anaemia, whilst serum ferritin levels below 40 ng/mL correlate with telogen effluvium in approximately 30% of premenopausal women[5]. Thyroid function tests, particularly thyroid stimulating hormone measurements, detect underlying thyroid disorders that affect hair growth cycles, with both hypothyroidism and hyperthyroidism contributing to diffuse hair thinning.
Despite their value, blood tests cannot diagnose the majority of hair loss conditions encountered clinically. Androgenetic alopecia, affecting 50% of men and 40% of women by middle age, typically presents with normal laboratory values despite significant hair loss[6]. Similarly, alopecia areata, traction alopecia, and early-stage scarring alopecias rarely demonstrate abnormal blood markers. Vitamin D deficiency, whilst associated with various hair disorders, lacks definitive causal evidence. The diagnostic sensitivity of blood tests for common hair loss conditions remains below 25%, necessitating comprehensive physical examination and trichoscopic evaluation for accurate diagnosis. Normal ferritin levels and thyroid function don’t exclude significant hair loss pathology.
Female Pattern Hair Loss: Beyond Laboratory Values
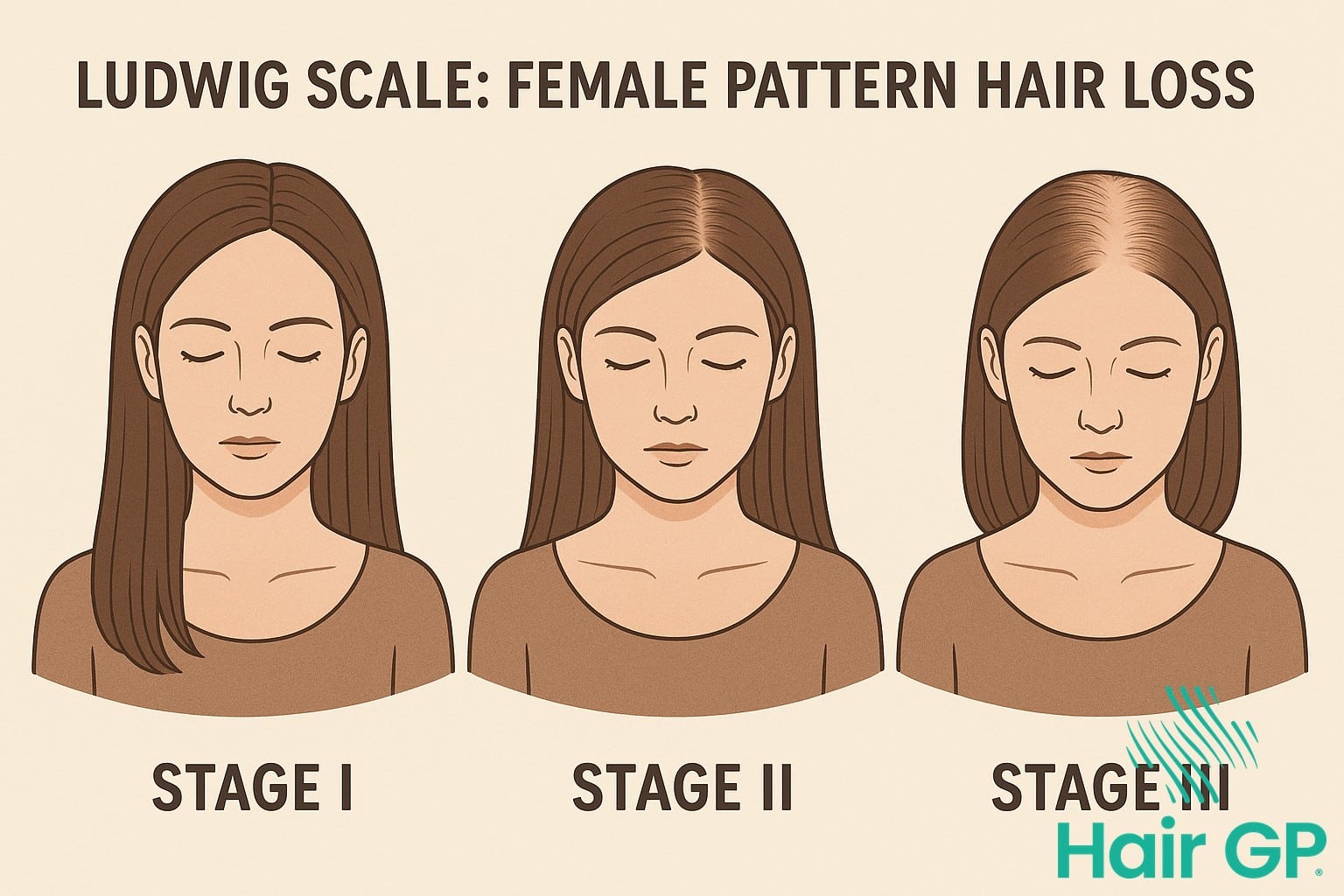
Female pattern hair loss affects approximately 40% of women by age 50, yet standard blood work typically reveals normal hormone levels despite visible hair thinning [7]. This hormonal paradox challenges conventional diagnostic approaches, as androgens often remain within normal ranges whilst follicles demonstrate heightened sensitivity to circulating hormones. The Ludwig scale provides clinical classification through three progressive stages: diffuse thinning with preserved frontal hairline (I), marked widening with decreased coverage (II), and extensive loss revealing scalp visibility (III) [8].
Central part widening assessment proves more reliable than laboratory values for diagnosis, particularly when evaluating hereditary hair loss patterns across generations. African American women may present differently, with central centrifugal scarring potentially masking underlying female pattern baldness. Family history evaluation reveals genetic predisposition in 70-80% of cases, though current genetic testing limitations cannot predict severity or treatment response. Clinical examination identifies characteristic miniaturisation patterns invisible to blood work, whilst photographic documentation captures progressive changes that hormonal assays miss. This clinical-focused approach enables earlier intervention with proven treatments like minoxidil before extensive follicular damage occurs.
Alopecia Areata: Immune Patterns Blood Work Can’t Detect
Despite alopecia areata being a well-established autoimmune condition, no specific blood test can confirm its diagnosis. Whilst white blood cells attack hair follicles in this disorder, these immune patterns remain localised to the scalp and cannot be detected through standard autoantibody panels or inflammatory markers[9]. The immune system dysfunction causing patchy hair loss occurs at the follicular level, where T-lymphocytes infiltrate the hair bulb without producing measurable systemic changes.
Clinical examination remains the gold standard for diagnosing areata, with characteristic features including exclamation mark hairs—broken strands that taper towards the scalp—surrounding patchy bald spots. These diagnostic signs, combined with the distinctive smooth, round patches and potential nail pitting, provide more reliable confirmation than any laboratory investigation[10]. The condition’s spontaneous regrowth patterns, often beginning with fine white hairs, further distinguish it from other autoimmune diseases affecting hair. This localised immune response explains why corticosteroid treatment targets the scalp directly rather than systemic immunosuppression.

Advanced Diagnostic Techniques: Scalp Biopsy and Trichoscopy
When blood tests and physical examination fail to establish a definitive hair loss diagnosis, advanced diagnostic techniques become essential. Scalp biopsy and trichoscopy provide microscopic insights that reveal pathological processes invisible to conventional laboratory tests, particularly crucial for diagnosing scarring alopecia conditions like lichen planopilaris.
Horizontal Versus Vertical Sectioning in Scalp Biopsy
The punch biopsy technique’s diagnostic yield depends significantly on sectioning orientation, with horizontal sections providing superior follicular density assessment compared to vertical processing [1]. This 4-millimetre procedure evaluates inflammatory infiltrate patterns throughout the follicular unit, revealing perifollicular fibrosis characteristic of scarring processes that dermoscopy alone cannot definitively confirm. Horizontal sectioning captures 20-30 follicles per specimen, enabling accurate quantification of terminal-to-vellus hair ratios essential for androgenetic alopecia staging [11].
Trichometric analysis using polarised light microscopy achieves 94% sensitivity in detecting hair shaft abnormalities when combined with fungal culture testing. While trichoscopy offers non-invasive visualization with 85% specificity for common alopecias, the microscope examination of biopsy specimens remains gold standard for ambiguous presentations requiring cellular-level evaluation beyond standard diagnostic tests.
Identifying the True Cause of Hair Loss Through Comprehensive Assessment
Diagnosing hair loss requires systematic integration of multiple assessment modalities, beginning with comprehensive medical history that explores family history of alopecia, recent stressors, medications, and dietary changes. The physical exam extends beyond the scalp, evaluating nail changes, skin manifestations, and body hair distribution patterns that suggest an underlying medical condition causing hair loss.
Trichoscopic findings provide crucial diagnostic clues that blood tests cannot capture—miniaturisation patterns distinguish androgenetic alopecia from telogen effluvium, whilst exclamation mark hairs indicate alopecia areata. Combining these visual markers with selective laboratory testing creates a diagnostic algorithm that identifies the underlying cause more reliably than isolated investigations.
Red flags during assessment include rapid progression, associated systemic symptoms, or atypical distribution patterns warranting extensive workup. This multimodal approach ensures accurate diagnosis and appropriate treatment planning, recognising that normal blood results don’t exclude treatable conditions. The synthesis of clinical findings ultimately determines whether the cause of hair loss is primarily structural, inflammatory, or systemic.
Treatment Planning Based on Scalp-Level Diagnosis
Accurate scalp-level diagnosis transforms treatment outcomes by matching interventions precisely to pathological findings. When physical examination reveals characteristic miniaturisation patterns of androgenetic alopecia, treatment plans incorporating finasteride or minoxidil achieve significantly higher success rates compared to empirical therapy [12]. Identifying follicular miniaturisation early enables timely intervention with Propecia or Rogaine before permanent damage occurs, potentially helping patients hair regrow in affected areas.
Inflammatory findings guide different protocols entirely. Active inflammation around follicles necessitates anti-inflammatory treatment before starting growth stimulants, whilst scarring patterns may indicate laser therapy or hair transplant as the only permanent solution. The degree of follicular damage visible on examination determines whether to start treatment conservatively or pursue aggressive combination therapy. Studies demonstrate that diagnosis-guided protocols can stop hair loss progression in over 85% of patients when implemented appropriately [13]. This targeted approach minimises unnecessary medication exposure whilst maximising therapeutic efficacy, reducing both treatment costs and potential side effects through precise intervention selection based on clinical findings.
Conclusion
Whilst blood tests provide essential baseline health information, achieving an accurate diagnosis of hair loss requires comprehensive evaluation beyond laboratory values. A qualified dermatologist or Hair Loss specialist performs detailed scalp examinations, dermoscopy assessments, and pull tests that reveal critical information about follicular health, inflammation patterns, and hair shaft integrity. This scalp level diagnosis uncovers what blood work can’t tell about hair loss, including miniaturisation patterns, follicular density changes, and early-stage conditions that standard testing misses.
To advocate for comprehensive evaluation, request specific diagnostic procedures during consultation: trichoscopy examination, standardised photography for progression monitoring, and detailed medical history assessment including medications and lifestyle factors. Seek practitioners who combine laboratory testing with advanced diagnostic techniques rather than relying solely on blood results. Schedule comprehensive hair loss evaluation with a Hair Loss Specialist who understands the complexity of hair disorders beyond hormonal parameters. Remember that effective treatment depends on accurate diagnosis—investing in thorough initial assessment saves time, prevents ineffective treatments, and leads to better outcomes for your hair health journey.
Frequently Asked Questions
Yes, many common hair loss conditions including androgenetic alopecia, alopecia areata, and telogen effluvium can present with entirely normal blood work. These conditions are diagnosed through physical examination, dermoscopy, and sometimes scalp biopsy rather than laboratory tests.
Physical examination techniques including the pull test, trichoscopy, dermoscopy, and scalp biopsy often provide more diagnostic value than blood tests. These methods directly visualize hair follicles, identify miniaturization patterns, and detect inflammatory changes invisible to laboratory testing.
Request comprehensive scalp examination when experiencing progressive hair loss despite normal blood work, patchy hair loss patterns, scalp symptoms like itching or pain, or when standard treatments aren’t working. Physical examination can reveal conditions that blood tests simply cannot detect.
References
- Geyfman M, Plikus MV, Treffeisen E, et al. Resting no more: re-defining telogen, the maintenance stage of the hair growth cycle. Biol Rev Camb Philos Soc. 2015;90(4):1179-96.
- Hoover E, Alhajj M, Flores JL. Physiology, Hair. StatPearls. 2021.
- Rudnicka L, Olszewska M, Waśkiel-Burnat A, Rakowska A. Trichoscopy in Hair and Scalp Disease. Dermatol Clin. 2018;36(4):421-430.
- Tosti A, Torres F. Dermoscopy in the diagnosis of hair and scalp disorders. Actas Dermosifiliogr. 2015;106(2):158-167.
- Trost LB, Bergfeld WF, Calogeras E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol. 2006;54(5):824-844.
- Piraccini BM, Alessandrini A. Androgenetic alopecia. G Ital Dermatol Venereol. 2014;149(1):15-24.
- Ramos PM, Miot HA. Female Pattern Hair Loss: a clinical and pathophysiological review. An Bras Dermatol. 2015;90(4):529-543.
- Herskovitz I, Tosti A. Female pattern hair loss. Int J Endocrinol Metab. 2013;11(4):e9860.
- Darwin E, Hirt PA, Fertig R, et al. Alopecia Areata: Review of Epidemiology, Clinical Features, Pathogenesis, and New Treatment Options. Int J Trichology. 2018;10(2):51-60.
- Strazzulla LC, Wang EHC, Avila L, et al. Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78(1):1-12.
- Stefanato CM. Histopathology of alopecia: a clinicopathological approach to diagnosis. Histopathology. 2020;76(1):6-23.
- Gupta AK, Mays RR, Dotzert MS, Versteeg SG, Shear NH, Piguet V. Efficacy of non-surgical treatments for androgenetic alopecia: a systematic review and network meta-analysis. J Eur Acad Dermatol Venereol. 2018;32(12):2112-2125.
- Adil A, Godwin M. The effectiveness of treatments for androgenetic alopecia: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(1):136-141.e5.