Introduction
The Mirena coil has become one of the most popular forms of long-acting birth control, offering women reliable contraception for up to five years. Yet amongst its many benefits, a persistent question troubles many users: what impact does this hormonal contraception have on their hair? For some women, the intrauterine device represents a solution to hormone-related hair problems, whilst others report concerning hair loss after insertion.
This debate isn’t simply about vanity. Hair health significantly impacts self-confidence and quality of life, making it a crucial consideration when choosing contraceptive methods. The Mirena coil releases a synthetic hormone called levonorgestrel directly into the uterus, with small amounts entering the bloodstream. This localised hormone delivery makes it an attractive option, but it can still influence hair growth patterns in sensitive individuals.
Understanding the relationship between Mirena and hair requires examining multiple perspectives. We’ll explore the science behind how this device works in your body and why hormones affect hair follicles differently in different women. You’ll discover real experiences from users who’ve noticed changes—both positive and negative—in their hair health. We’ll provide practical strategies for maintaining healthy hair whilst using Mirena, and discuss alternative options if hair concerns become significant.
Whether you’re considering Mirena, currently using it, or experiencing hair changes, this comprehensive guide offers evidence-based insights to help you make informed decisions about your reproductive health and hair wellbeing.
Key Takeaways – TL/DR
- The Mirena coil releases synthetic progesterone that can trigger hair loss in some women, especially those predisposed to hormonal hair changes
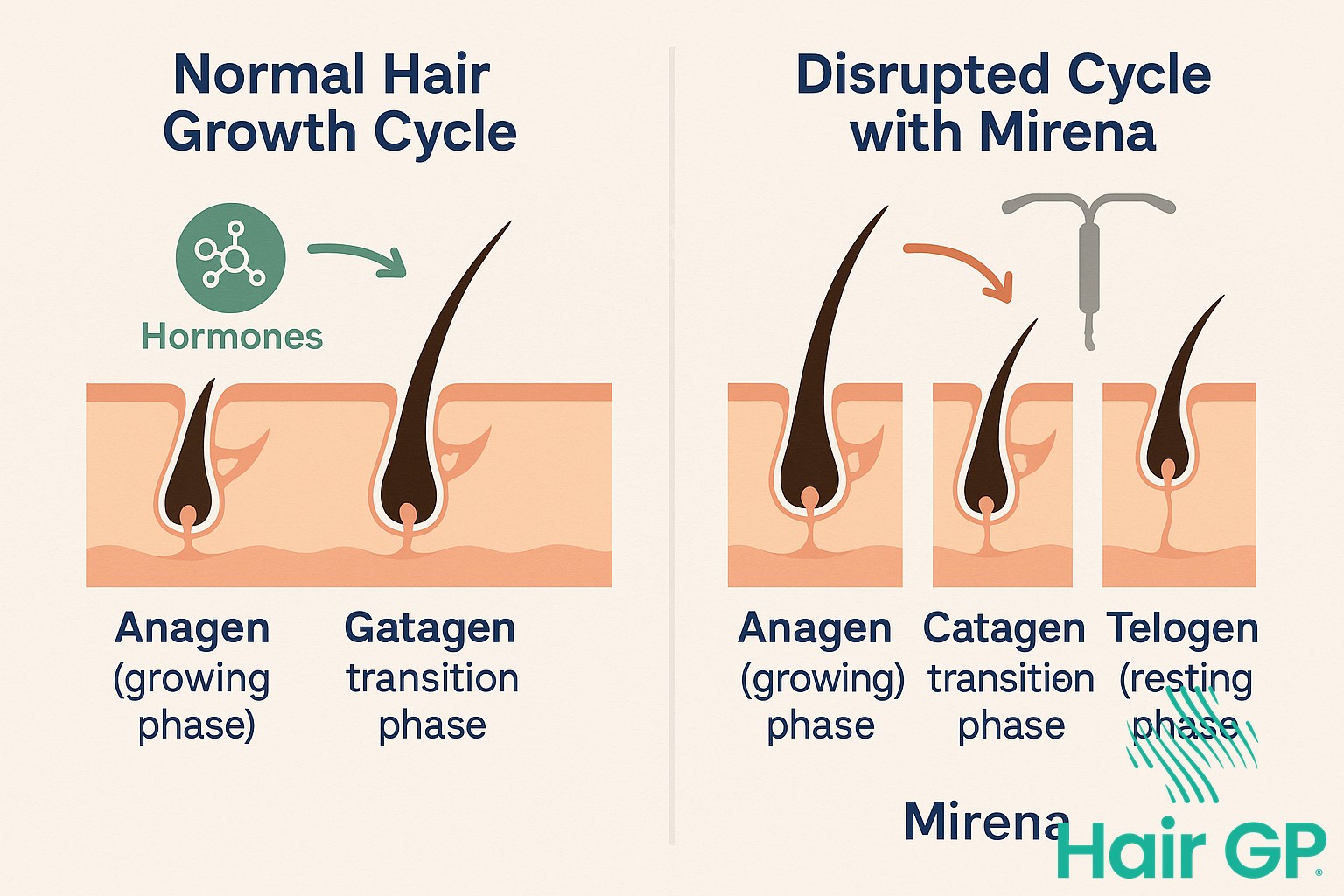
- Hair loss typically occurs 3-6 months after insertion due to disrupted hair growth cycles
- Not all women experience hair loss – some report improved hair health after Mirena insertion
- Hair loss is usually temporary and reversible after removal, though recovery can take 6-12 months
- Alternative contraceptive options exist for women concerned about hair-related side effects
Understanding the Mirena Coil: How It Works in Your Body
The Mirena coil stands as a revolutionary advancement in hormonal contraception, offering women a long-term, reversible birth control option that requires minimal maintenance. This small, T-shaped intrauterine device measures just 32mm by 32mm and fits comfortably within the uterus, where it provides continuous protection against pregnancy for up to five years.
At the heart of the Mirena IUD’s effectiveness lies its innovative hormone delivery system. The device contains a reservoir of 52mg of levonorgestrel, a synthetic progestogen that releases slowly and steadily into the uterine cavity. This localised hormone release creates multiple contraceptive mechanisms: it thickens cervical mucus to prevent sperm penetration, inhibits sperm movement and function within the uterus and fallopian tubes, and in some women, prevents ovulation. The initial release rate of approximately 20 micrograms per day gradually decreases over time, maintaining therapeutic levels throughout its five-year lifespan.
Clinical studies demonstrate the exceptional reliability of this hormonal contraception method. The Mirena boasts a failure rate of less than 1%, making it one of the most effective reversible birth control options available. Unlike daily oral contraceptives, the intrauterine device eliminates the risk of user error, providing consistent protection without requiring daily attention or monthly prescriptions.
Beyond its primary role in preventing pregnancy, healthcare providers increasingly recommend the Mirena for managing various gynaecological conditions. Women suffering from heavy menstrual bleeding often experience significant relief, with many reporting lighter periods or complete amenorrhoea. The steady levonorgestrel release helps stabilise the endometrial lining, reducing excessive bleeding that can lead to anaemia and impact quality of life. Additionally, the device proves beneficial for managing endometriosis symptoms, providing localised hormone therapy that can reduce pain and inflammation associated with this chronic condition.
The dual nature of the Mirena as both contraception and therapeutic treatment makes it particularly appealing to women seeking comprehensive reproductive health management. Its high concentration of hormone delivery directly to the uterus means lower systemic absorption compared to oral contraceptives, potentially reducing some hormonal side effects. However, as with any hormonal contraception, individual responses vary significantly, and some women may experience changes in various body systems, including potential effects on hair growth patterns that warrant careful consideration and monitoring.

The Science Behind Mirena and Hair Loss
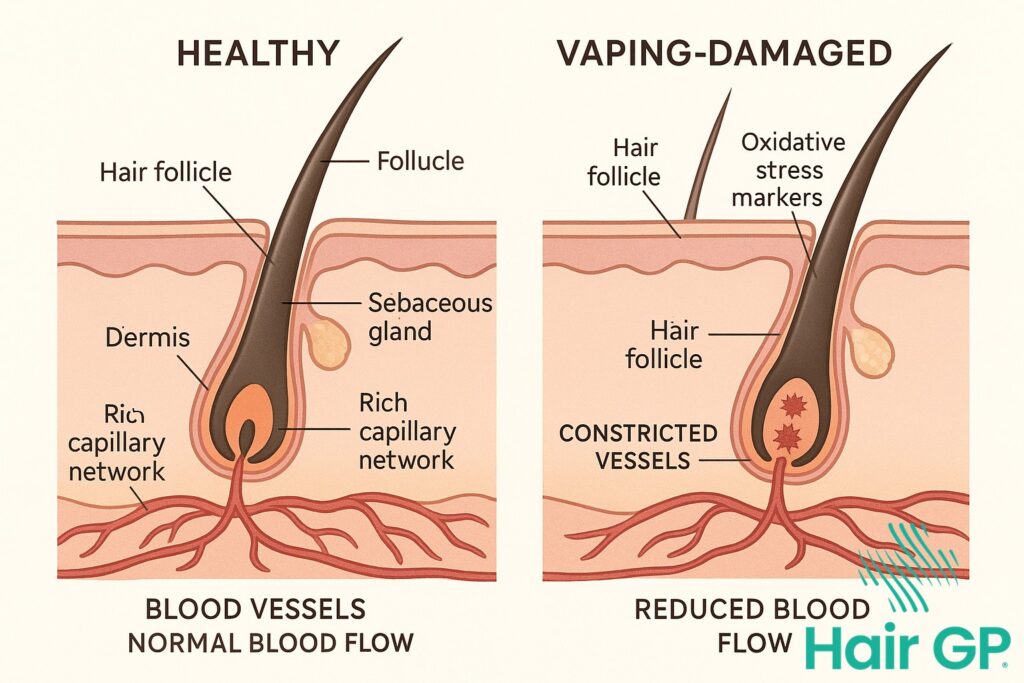
The biological mechanisms linking Mirena to hair loss centre on how synthetic hormones disrupt normal follicular function. Levonorgestrel, the synthetic progestogen in Mirena, possesses androgenic properties that can trigger hair thinning in susceptible women by altering the delicate hormonal balance required for healthy hair growth cycles.
How Hormones Control Hair Growth
Hair growth depends on a complex interplay between oestrogen, progesterone, and androgens, with each hormone playing distinct roles in follicular health. Oestrogen promotes the anagen (growth) phase of hair cycles, whilst progesterone helps maintain hair thickness and prevents excessive shedding [1]. Natural progesterone acts as an anti-androgen, protecting hair follicles from the miniaturising effects of dihydrotestosterone (DHT).
However, synthetic hormones differ significantly from their natural counterparts. Levonorgestrel, despite being classified as a progestogen, exhibits substantial androgenic activity—approximately three times stronger than natural progesterone [2]. This androgenic property means it can bind to androgen receptors in hair follicles, potentially triggering the same miniaturisation process seen in androgenetic alopecia.
The scalp contains numerous androgen receptors, particularly in the frontal and crown regions. When levonorgestrel binds to these receptors, it can shorten the anagen phase and prolong the telogen (resting) phase, leading to progressive hair thinning. Additionally, some women demonstrate heightened hormone sensitivity, meaning even small amounts of synthetic hormones can trigger significant follicular changes.
Why Some Women Are More Affected
Genetic predisposition plays a crucial role in determining who experiences Mirena-related hair loss. Women with a family history of androgenetic alopecia possess more sensitive follicular androgen receptors, making them particularly vulnerable to levonorgestrel’s androgenic effects. These genetic variations influence how efficiently the body converts testosterone to DHT and how strongly follicles respond to androgenic stimulation.
Existing hormonal imbalances significantly increase susceptibility. Women with polycystic ovary syndrome (PCOS), thyroid disorders, or naturally elevated androgen levels often experience more pronounced hair loss with Mirena. Thyroid hormones particularly influence hair growth cycles, and any disruption—whether from hypothyroidism or hyperthyroidism—can amplify hormonal contraceptive effects on hair.
Nutritional status also determines hair loss severity. Iron deficiency, common in menstruating women, weakens hair structure and exacerbates hormonally-induced shedding. Similarly, deficiencies in vitamin D, B vitamins, and zinc compromise the follicle’s ability to withstand hormonal fluctuations. Women with optimal nutritional status often demonstrate greater resilience against Mirena-related hair changes.
Age represents another critical factor. Perimenopausal women, already experiencing declining oestrogen levels, may find that Mirena’s androgenic effects become more pronounced without sufficient oestrogenic protection. Conversely, younger women with robust oestrogen production might experience minimal hair changes despite identical levonorgestrel exposure.
Understanding these mechanisms helps explain why Mirena affects women so differently, with some experiencing significant hair loss whilst others notice no changes whatsoever.
When the mirena can help Hair Loss
While some women worry that hormonal contraception might trigger hair loss, the Mirena coil can actually help in certain cases — particularly when heavy periods are a contributing factor. One of the most common causes of diffuse hair shedding in women is iron deficiency, often linked to heavy menstrual bleeding over time. When someone is consistently losing more blood than their body can comfortably replace each month, their iron stores drop, and this can quietly start to affect hair growth.
In women with very heavy periods, the Mirena can reduce bleeding dramatically — and in many cases, stop periods altogether. This can give the body a chance to restore iron levels and stop the cycle of monthly depletion. I’ve seen women who were previously iron-deficient and experiencing hair loss regain not just their energy, but noticeable improvements in their hair over time, once their iron stores were rebuilt and their periods were under control.
If you’re experiencing hair thinning alongside heavy periods, it’s worth speaking to your GP about checking your iron levels with a simple blood test. Iron deficiency can be subtle and develop slowly, so even if your levels aren’t low enough to cause anaemia, they could still be low enough to affect your hair. For some women, addressing the underlying cause of heavy bleeding — whether through the Mirena coil or other treatment options — can make a real difference. Every case is individual, so it’s important to build a plan that’s right for your body, symptoms, and future goals.
Another possible benefit of the Mirena for hair lies in the way it delivers hormones. Unlike some contraceptives that create hormonal ups and downs, the Mirena releases a low, steady dose of progestogen directly into the uterus. For women who are particularly sensitive to hormonal fluctuations, this more stable environment may help reduce hair shedding triggered by hormonal shifts — especially around the time of ovulation or menstruation. Additionally, by easing symptoms like pain and heavy bleeding, the Mirena can help improve overall wellbeing. Feeling physically better often leads to reduced stress, improved sleep, and better energy — all of which can indirectly support healthier hair growth by giving the body a chance to recover and rebalance.

Managing Hair Health with Mirena: Practical Solutions
Managing hair health whilst using Mirena requires a comprehensive approach that addresses both nutritional support and practical care strategies. Research demonstrates that adequate nutrition plays a crucial role in maintaining healthy hair growth, particularly when hormonal contraceptives may be affecting follicle function. Iron deficiency remains one of the most common nutritional causes of hair loss in women, with studies showing that ferritin levels below 70 ng/mL can impair hair regrowth [3]. Women experiencing hair changes with Mirena should consider having their iron stores evaluated, particularly if they also experience heavy periods before insertion or other symptoms like fatigue.
Beyond iron, several other nutrients support scalp health and hair follicle function. Vitamin D receptors are present in hair follicles, and deficiency has been linked to various forms of alopecia [4]. Supplementation with 1000-2000 IU daily may benefit women with low levels, though testing should guide dosing. B-complex vitamins, particularly B12, support keratin production, whilst zinc deficiency can disrupt the hair growth cycle. A balanced diet rich in lean proteins, omega-3 fatty acids, and colourful vegetables provides the foundation for hair health, though targeted supplementation may be warranted based on individual needs.
Practical hair care becomes especially important when managing Mirena-related changes. Gentle handling reduces mechanical stress on potentially vulnerable hair. This includes using wide-toothed combs on wet hair, avoiding tight hairstyles that pull on the scalp, and limiting heat styling to prevent additional damage. Scalp massage with light pressure can improve circulation without causing trauma. When washing, lukewarm water and sulphate-free shampoos help maintain the scalp’s natural protective barrier. Some women find that reducing washing frequency to 2-3 times weekly helps preserve natural oils that protect hair shafts.
Stress management deserves particular attention, as cortisol elevation can compound hormonal effects on hair follicles. Regular exercise, adequate sleep, and stress-reduction techniques like meditation or yoga may help minimise hair loss. Interestingly, some women report that managing other Mirena side effects, such as weight gain or changes in libido, through lifestyle modifications also positively impacts their hair health.
Medical consultation becomes necessary when hair loss is rapid, patchy, or accompanied by scalp symptoms like burning or itching. Women should also seek evaluation if hair loss persists beyond six months or significantly impacts quality of life. This is particularly important for those using Mirena for conditions like endometriosis, where switching contraceptives requires careful consideration. A medical consultation can help determine whether hair changes are solely Mirena-related or if other factors contribute. Blood tests evaluating thyroid function, nutritional status, and androgen levels can guide treatment decisions and determine whether Mirena removal or additional interventions are warranted.

Making Your Decision: Alternatives and Considerations
When weighing up the Mirena IUD against other contraceptive options, understanding your individual risk factors for hair loss becomes crucial. Women with a family history of androgenetic alopecia or those who’ve experienced hair thinning with birth control pills may want to consider non-hormonal alternatives. The copper IUD offers similar long-term protection without synthetic hormones, though it may cause heavier periods—a trade-off some women find worthwhile to avoid potential hair loss.
For those requiring hormonal contraception, options vary in their androgenic activity. Combined oral contraceptives containing ethinylestradiol paired with low-androgenic progestins like drospirenone or desogestrel may pose less risk to hair health than the levonorgestrel in Mirena. However, these require daily compliance and don’t offer the ‘fit and forget’ convenience of having a coil fitted. Also combined oral contraceptives can put your risk of blood clots up so this needs to be carefully considered by you and your Doctor in choosing the best method.
Partners willing to share contraceptive responsibility might consider barrier methods or vasectomy for permanent protection. While less convenient than hormonal methods, these eliminate concerns about systemic side effects entirely. Natural family planning methods, though requiring dedication and regular cycles, appeal to women prioritising hormone-free options.
Discussing your concerns openly with healthcare providers proves essential. Bring your family history, previous experiences with hormonal contraception, and current hair health to the consultation. Ask about the specific progestin types in different contraceptives and their androgenic ratings. Request information about typical timelines for side effects and what monitoring they recommend.
The decision ultimately requires balancing multiple factors: effectiveness at preventing pregnancy, convenience, reversibility, and potential side effects. For women with existing hair concerns or genetic predisposition to hair loss, the slight risk may outweigh Mirena’s benefits. Conversely, those without risk factors who struggle with pill compliance or want reliable long-term protection whilst maintaining future fertility might find Mirena ideal.
Remember that contraceptive experiences vary significantly between individuals. What triggers hair loss in one woman may cause no issues in another. Creating a personalised risk-benefit analysis with your healthcare provider, considering your unique circumstances and priorities, ensures you make the most informed choice for your body and lifestyle.
Conclusion
The relationship between the Mirena coil and hair loss represents a complex interplay of hormonal factors that affects each woman differently. Whilst some experience significant thinning after having their Mirena fitted, others enjoy this form of contraception without any impact on their hair health. This individual variation underscores the importance of personalised healthcare decisions when choosing birth control methods.
Understanding that hormonal contraceptives can potentially trigger hair changes empowers women to make informed choices. For those who experience hair loss but wish to continue with Mirena due to its effective contraception and other benefits, various management strategies exist. From targeted nutritional support to specialised hair care routines, many women successfully maintain their hair health whilst benefiting from this long-acting contraceptive.
Ultimately, the decision to use or continue with the Mirena coil should involve careful consideration of personal priorities, medical history, and quality of life factors. Open communication with healthcare providers ensures that any hair-related concerns receive appropriate attention and that alternative birth control options are explored when necessary. Remember that hair loss, when it occurs, is typically reversible, offering reassurance to those navigating this challenging side effect.
Frequently Asked Questions
Most women who experience hair loss with Mirena notice it beginning 3-6 months after insertion. This timing coincides with the telogen effluvium phase, where hair follicles prematurely enter the resting phase due to hormonal changes.
Yes, in most cases hair will regrow after Mirena removal. Recovery typically takes 6-12 months as hormone levels normalize and hair follicles return to their normal growth cycle. Some women see improvement sooner with proper nutrition and hair care.
While you can’t completely prevent hormonally-triggered hair loss, you can minimize it through proper nutrition (especially iron and B vitamins), gentle hair care, stress management, and scalp health maintenance. Vitamin D and zinc are also fantastic for hair.
Yes, women with a family history of hormonal hair loss, existing thyroid conditions, PCOS, or previous sensitivity to hormonal birth control are at higher risk. Those who experienced postpartum hair loss may also be more susceptible.
References
- Grymowicz M, Rudnicka E, Podfigurna A, Napierala P, Smolarczyk R, Smolarczyk K et al.. Hormonal Effects on Hair Follicles. Int J Mol Sci. 2020. PMID: 32731328
- Herskovitz I, Tosti A. Female pattern hair loss. Int J Endocrinol Metab. 2013. PMID: 24719635
- Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002. PMID: 12190640
- Amor KT, Rashid RM, Mirmirani P. Does D matter? The role of vitamin D in hair disorders and hair follicle cycling. Dermatol Online J. 2010. PMID: 20178699