Introduction
Hair loss affects millions of people worldwide, yet the way it manifests can vary significantly between men and women. Understanding these differences is crucial for effective diagnosis and treatment, which is why medical professionals rely on specialised classification systems. The Ludwig Scale vs. Norwood Scale comparison represents the fundamental distinction in how we assess and categorise androgenetic alopecia across genders.
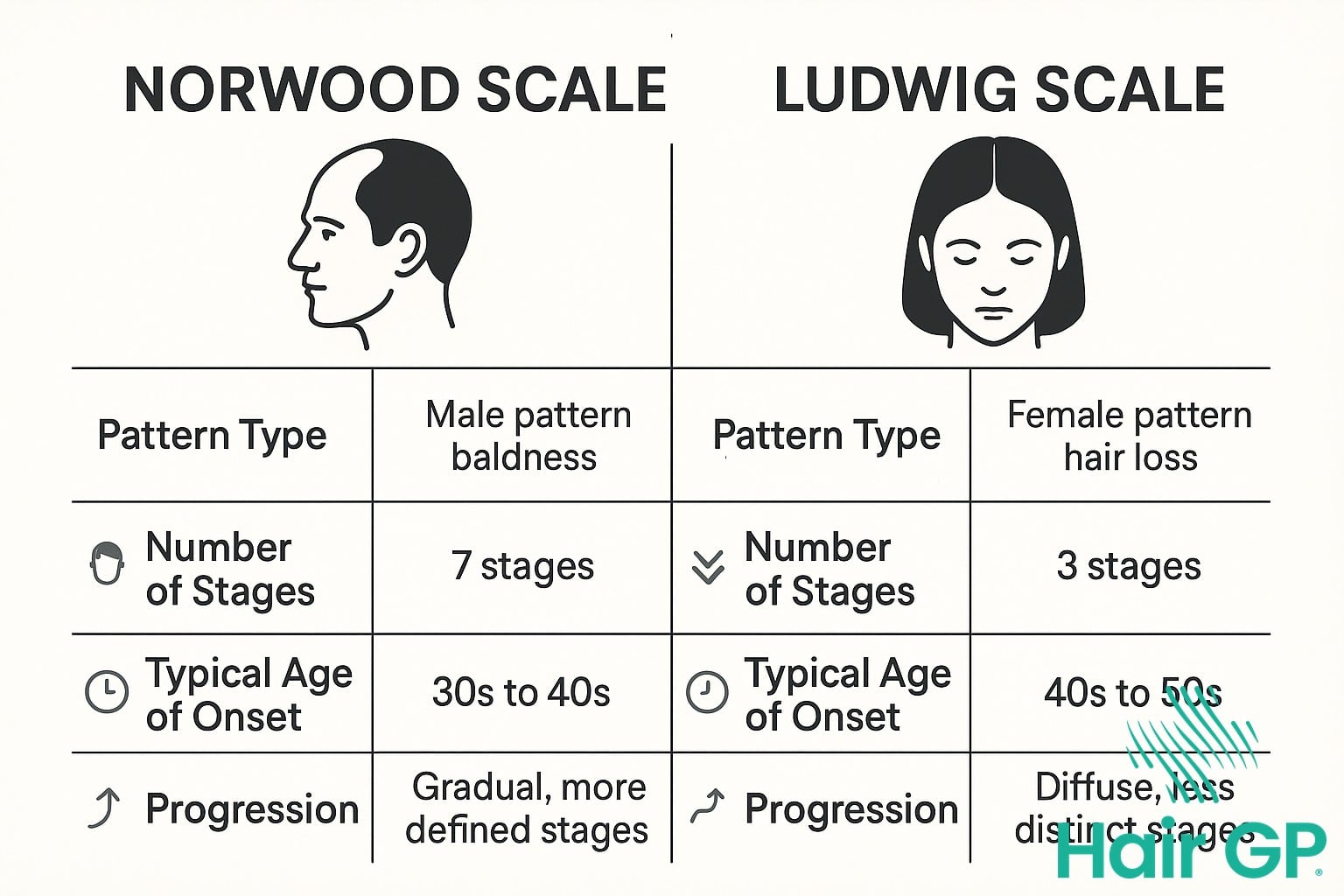
Whilst male pattern baldness typically follows a predictable pattern of receding hairlines and crown thinning, female hair loss presents quite differently, often appearing as diffuse hair thinning across the scalp. These distinct patterns led to the development of two separate classification systems: the Norwood Scale for men and the Ludwig Scale for women. Each system provides a standardised framework that helps healthcare providers evaluate the severity of hair loss and develop appropriate treatment strategies.
This comprehensive guide will explore how these classification systems work, examining the specific stages within each scale and what they mean for individuals experiencing hair loss related symptoms. We’ll delve into the biological and hormonal factors that create these gender-specific patterns, helping you understand why men and women experience androgenetic alopecia so differently. Additionally, we’ll review the latest evidence-based treatment options available for both genders, discussing how therapy selection varies based on your classification within these scales. Whether you’re personally experiencing hair thinning or seeking to understand these conditions better, this article provides the essential knowledge needed to navigate the complex landscape of pattern hair loss.
Key Takeaways – TL/DR
- The Norwood Scale classifies male pattern baldness in 7 stages, focusing on receding hairlines and crown thinning
- The Ludwig Scale identifies female hair loss in 3 main grades, emphasizing diffuse thinning while maintaining the frontal hairline
- Male and female pattern hair loss differ in progression patterns due to hormonal variations and genetic factors
- Both scales help determine appropriate hair loss treatments including topical minoxidil, finasteride, and other interventions
- Early identification using these scales leads to more effective treatment outcomes for both men and women
Understanding Hair Loss Classification Systems
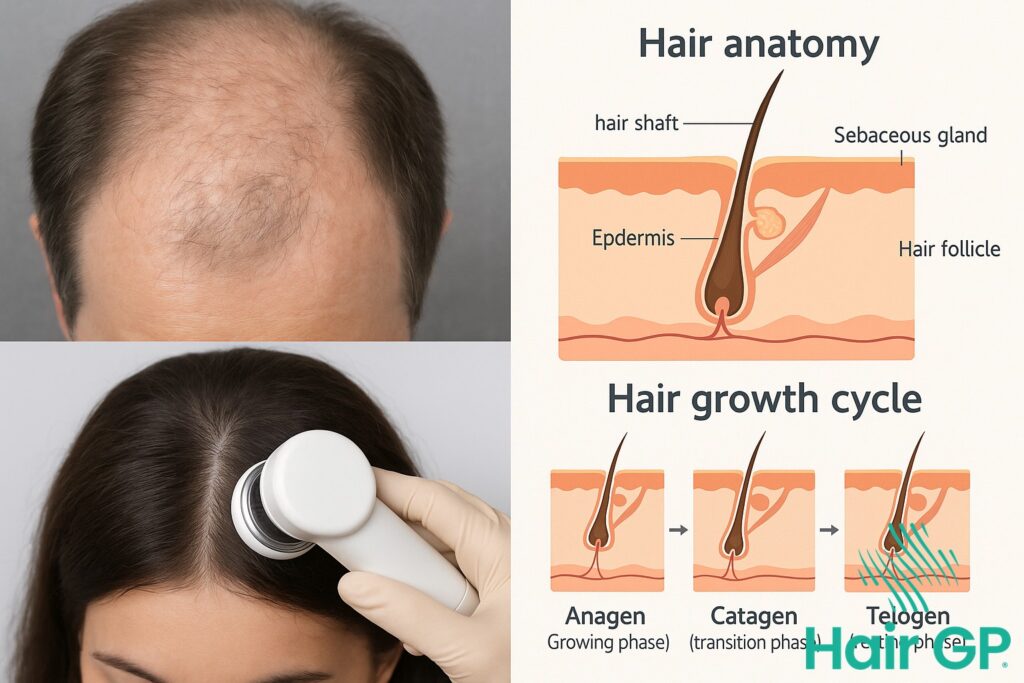
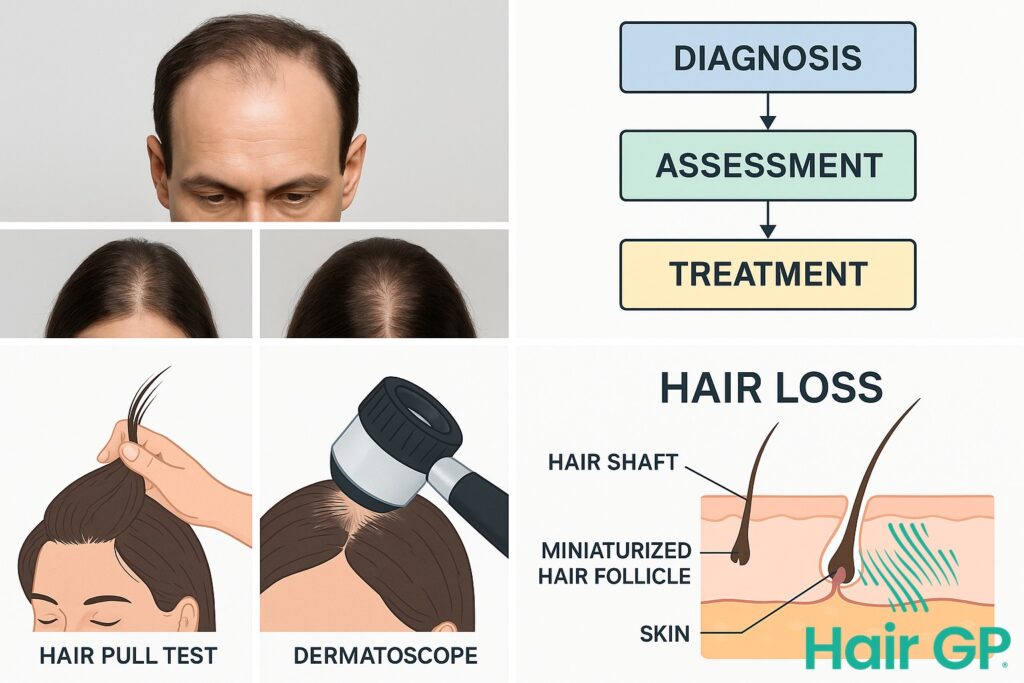
Hair loss classification systems serve as essential diagnostic tools that enable medical professionals to accurately assess and monitor the progression of alopecia in patients. These standardised scales provide a common language for healthcare providers worldwide, allowing them to determine the severity and pattern of baldness with precision. By establishing consistent criteria for evaluation, these systems facilitate communication between specialists and ensure patients receive appropriate treatment recommendations based on their specific condition.
The development of these classification systems emerged from the medical community’s recognition that hair loss presents in distinct patterns requiring systematic categorisation. In the mid-20th century, pioneering dermatologists observed that androgenetic alopecia manifested differently across populations, prompting the creation of gender-specific scales. These groundbreaking tools transformed how physicians approach hair follicle deterioration, moving from subjective assessments to objective, reproducible measurements that could track changes over time.
Modern medical practice relies heavily on these classification systems to develop personalised treatment strategies. When specialists can accurately categorise a patient’s hair loss pattern, they can better predict disease progression and select the most effective interventions. This systematic approach proves particularly valuable when prescribing hair loss medications, as different stages and patterns may respond differently to various therapeutic options. The scales also help establish realistic expectations for treatment outcomes and enable meaningful comparison of results across clinical studies.
Beyond their clinical applications, these classification systems empower patients by providing a framework for understanding their condition. Rather than experiencing anxiety about undefined changes, individuals can track their progression using established benchmarks. This knowledge facilitates informed discussions with healthcare providers and helps patients make educated decisions about when to seek treatment and which options might best suit their particular situation.
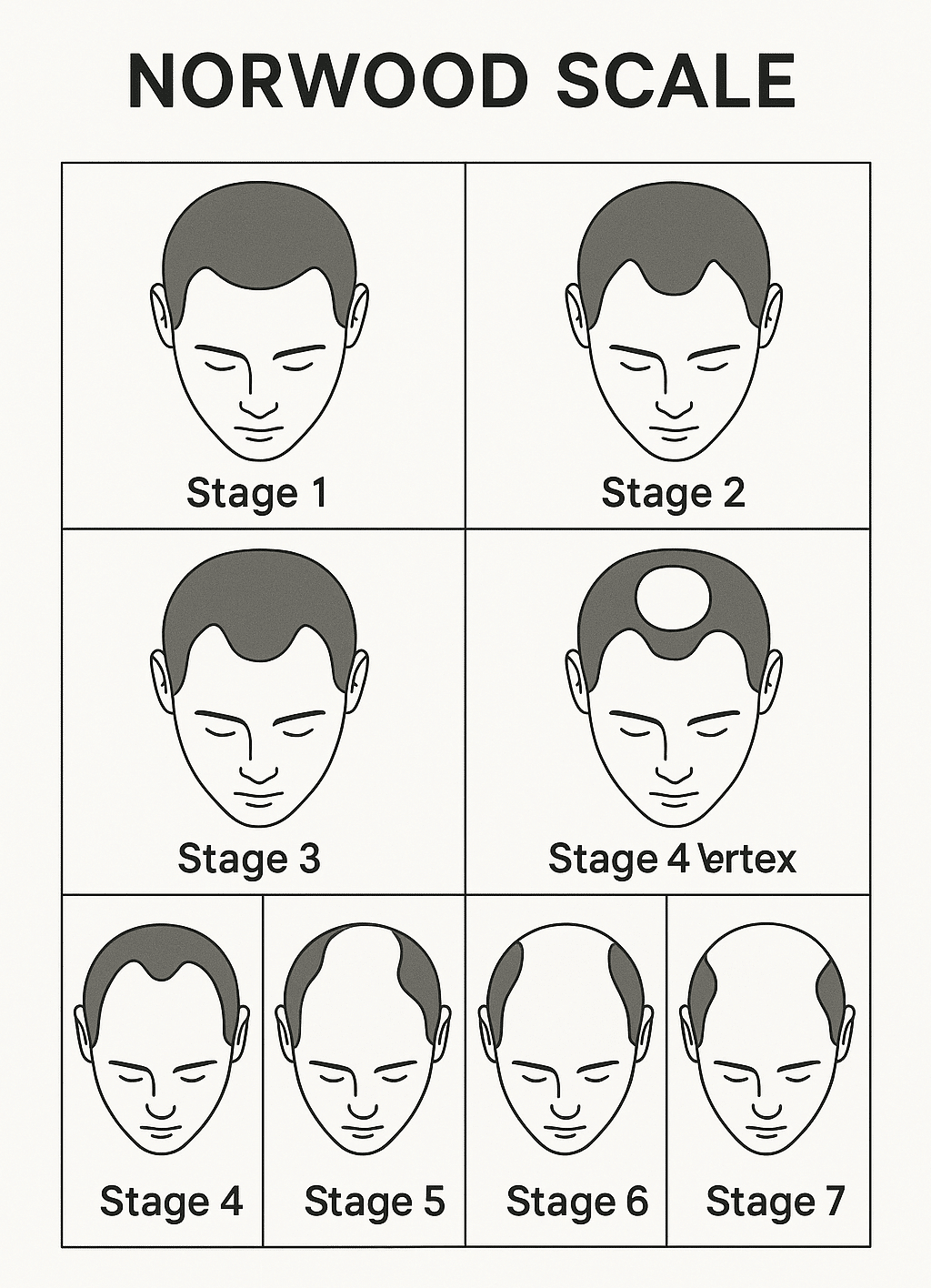
The Norwood Scale: Male Pattern Baldness Classification
The Norwood-Hamilton Scale serves as the gold standard for classifying male pattern baldness, providing a systematic approach to understanding how hair loss progresses in men. This seven-stage classification system, developed by Dr O’Tar Norwood in 1975 as a modification of Hamilton’s original work, helps clinicians assess the severity of androgenetic alopecia and determine appropriate treatment strategies [1].
Stages 1-3: Early Hair Loss
Stage 1 represents minimal hair recession with no significant visible hair loss, often indistinguishable from a mature hairline. Most men at this stage show little to no concern about balding, as the hairline remains relatively intact.
Stage 2 introduces the characteristic M-shaped pattern as the hairline begins receding at the temples. This subtle change affects approximately 25% of men by age 30, marking the initial signs of male pattern baldness [2]. The frontal hairline typically recedes 1-2 centimetres from its original position.
Stage 3 marks the first clinically significant level of hair loss, with deep temporal recession creating pronounced balding at the temples. Men reaching this stage often seek treatment options to prevent further progression, as the hair loss becomes noticeable to others. A variant called Stage 3 Vertex includes additional thinning at the crown whilst maintaining the frontal hairline.
Stages 4-7: Advanced Hair Loss
Stage 4 introduces substantial crown balding alongside continued frontal recession. The band of hair separating the two balding areas becomes narrower, and DHT continues affecting susceptible follicles. This stage often motivates men to actively treat male pattern baldness through medical interventions.
Stages 5 and 6 represent progressive merging of the crown and frontal balding areas. In Stage 5, the connecting hair bridge remains but becomes significantly thinner. Stage 6 shows complete merging, leaving only hair on the sides and back of the scalp. Male sex hormones continue driving follicular miniaturisation throughout these stages.
Stage 7 represents the most extensive hair loss pattern, with only a horseshoe-shaped band of hair remaining around the sides and back of the head. This residual hair typically resists DHT effects due to different genetic programming. Whilst treatment options remain available, restoration becomes more challenging at this advanced stage.
Understanding where one falls on the Norwood Scale enables informed decisions about intervention timing and realistic expectations for treatment outcomes in managing male pattern baldness.
The Ludwig Scale: Female Pattern Hair Loss Classification
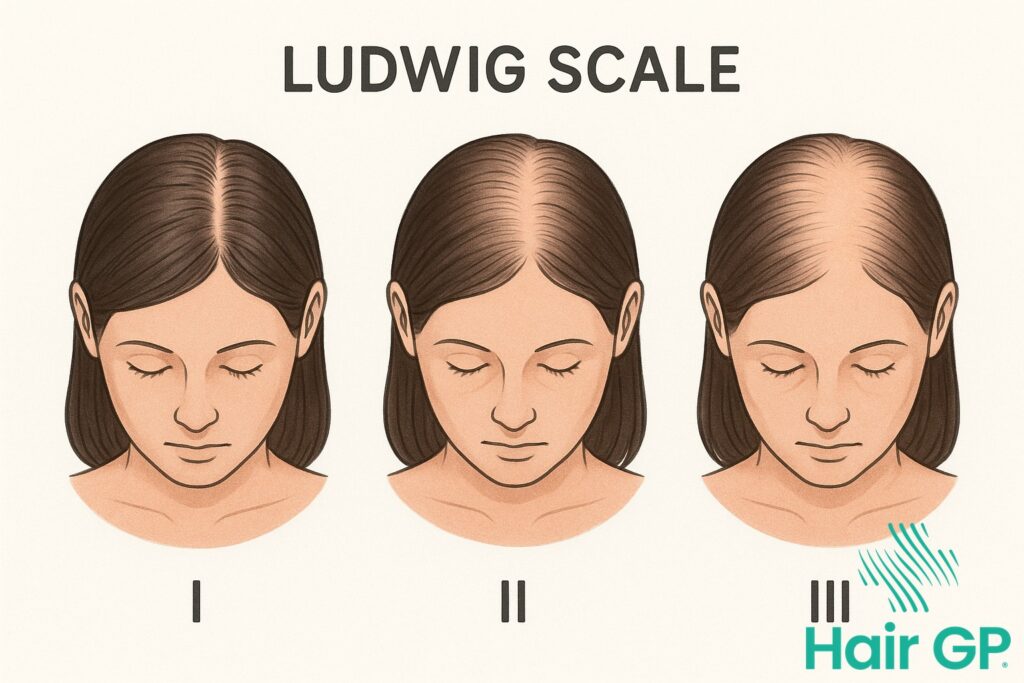
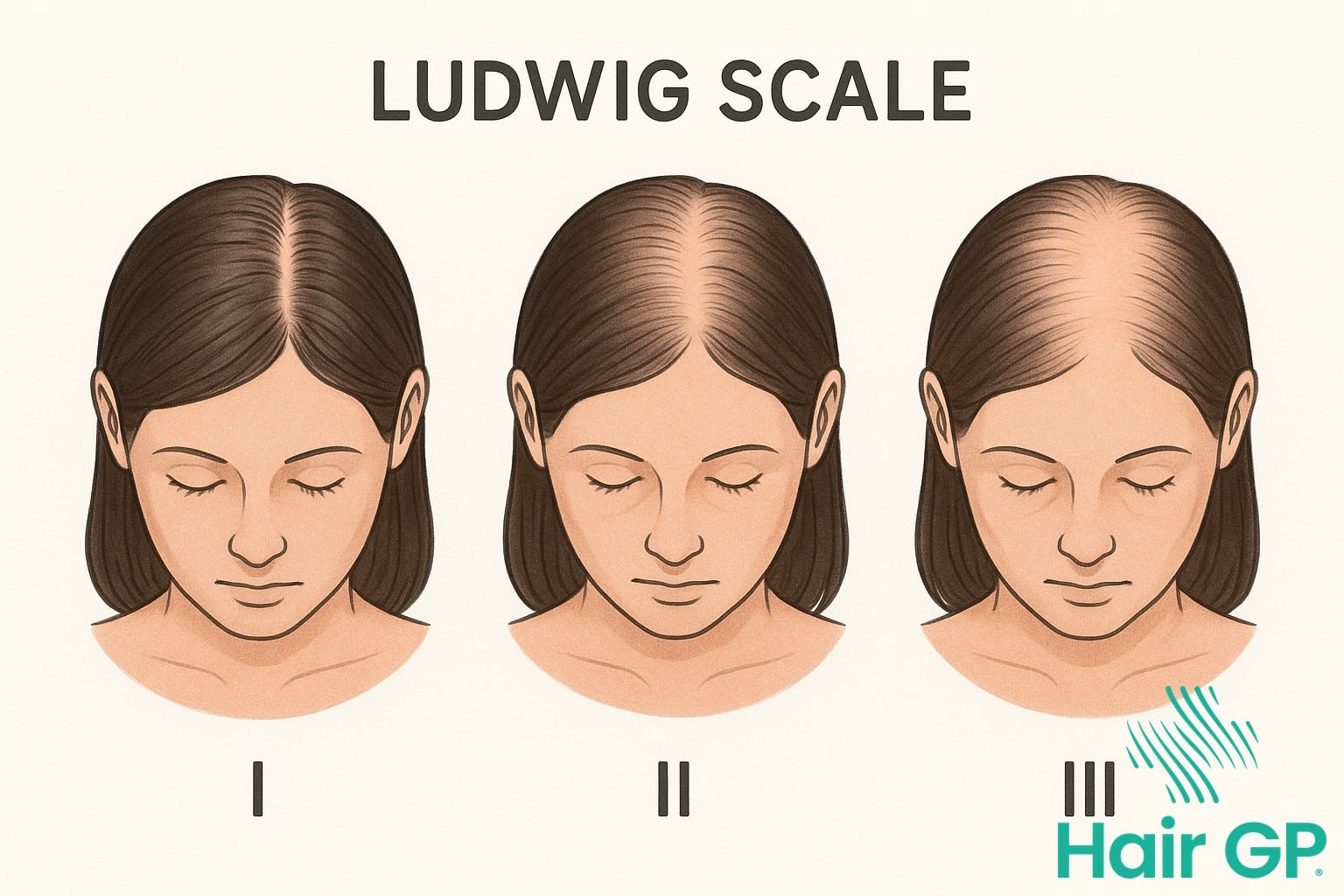
The Ludwig Scale represents the primary classification system for evaluating female pattern hair loss, providing clinicians with a standardised method to assess the unique presentation of hair thinning in women. Unlike male pattern baldness which typically follows a receding hairline pattern, female pattern hair loss manifests as diffuse thinning across the crown whilst preserving the frontal hairline. This distinctive pattern requires a specialised grading system that accurately reflects the progressive nature of hair loss experienced by women.
Grade I: Mild Thinning
Grade I represents the earliest stage of female pattern hair loss, characterised by minimal visible hair thinning that may be barely perceptible to casual observation. The most notable feature involves a gradual widening of the central part line, where the scalp becomes slightly more visible when hair is parted in the middle. Despite this central thinning, the frontal hairline remains completely preserved, maintaining its original position and density. Women experiencing Grade I often notice increased shedding during hair washing or brushing, though the overall volume appears relatively normal. The hair follicles in affected areas begin showing signs of miniaturisation, producing progressively finer strands that contribute to the perception of reduced density.
Grades II and III: Progressive Thinning
Grade II marks a significant progression where hair thinning becomes noticeably apparent, particularly around the crown region. The central part widens considerably, revealing more scalp visibility that extends laterally from the midline. This stage affects a broader area of the crown whilst still maintaining frontal hairline integrity. The diffuse pattern throughout the crown creates an increasingly transparent appearance where individual hair strands fail to provide adequate scalp coverage. Grade III represents the most severe classification, involving extensive scalp visibility across the entire crown region. At this advanced stage, the affected area may extend from the frontal region to the vertex, though some peripheral hair density typically remains. The human hair follicles undergo substantial miniaturisation, producing vellus-like hairs that provide minimal coverage. This progression differs significantly from telogen effluvium, which causes temporary diffuse shedding rather than the permanent follicular changes seen in female pattern hair loss. Understanding these distinctions enables appropriate treatment selection and realistic expectation setting for affected women.
Key Differences Between Ludwig and Norwood Scales
The fundamental distinction between the Ludwig and Norwood scales lies in their recognition that male pattern baldness and female hair loss manifest through entirely different mechanisms and patterns. Whilst the Norwood scale tracks the systematic recession of hairlines and crown thinning characteristic of male androgenetic alopecia, the Ludwig scale addresses the diffuse thinning pattern unique to women, highlighting why separate classification systems remain essential for accurate diagnosis and treatment planning.
Male hair loss patterns typically follow a predictable progression, beginning at the temples and advancing towards the crown of the head. This pattern reflects the sensitivity of specific follicles to dihydrotestosterone (DHT), which disrupts the normal hair growth cycle. In contrast, female pattern hair loss presents as overall thinning across the scalp whilst maintaining the frontal hairline, creating a widening part rather than distinct bald patches. This difference stems from variations in androgen receptor distribution and hormonal influences between sexes.
The progression rates between these patterns vary significantly throughout different life stages. Male pattern baldness often begins earlier, with noticeable changes occurring from the late teens or early twenties, and can advance rapidly over a relatively short period. Women typically experience gradual thinning that accelerates during hormonal transitions, particularly around menopause when oestrogen levels decline. Research indicates that whilst 50% of men show visible hair loss by age 50, women often maintain relatively stable patterns until hormonal shifts trigger more pronounced changes.
These distinct patterns necessitate different classification approaches. The Norwood scale’s seven stages capture the progressive nature of male pattern baldness, from temporal recession to extensive crown involvement. The Ludwig scale’s three-stage system, however, focuses on density reduction rather than pattern changes, reflecting how women rarely develop completely bald areas. This fundamental difference influences treatment strategies, as interventions must target either pattern-specific loss in men or diffuse thinning in women, requiring practitioners to understand both scales for comprehensive patient care and appropriate therapeutic recommendations based on the specific type of hair loss patterns presented.
Biological Factors Behind Gender-Specific Hair Loss
The biological mechanisms underlying gender-specific hair loss patterns reflect fundamental differences in hormonal profiles and genetic susceptibility between men and women. Whilst both sexes experience hair loss related to androgens, the manifestation and severity differ significantly due to distinct physiological factors.
Dihydrotestosterone (DHT), a potent derivative of testosterone, plays a central role in pattern hair loss for both genders[3]. This hormone binds to receptors within the hair follicle, triggering a process called miniaturisation where follicles progressively shrink and produce thinner, shorter hairs. Male sex hormones, particularly testosterone and DHT, exist at substantially higher levels in men, explaining the more aggressive and extensive hair loss patterns typically observed in male pattern baldness.
Women possess several protective biological factors that modify their hair loss presentation. Lower baseline androgen levels combined with the presence of aromatase enzymes, which convert androgens to oestrogens within the scalp, provide partial protection against follicular miniaturisation[4]. Additionally, women’s hair follicles demonstrate reduced sensitivity to DHT compared to men’s, particularly in the frontal hairline region, which explains why women typically maintain their anterior hairline whilst experiencing diffuse central thinning.
Several risk factors influence the development and progression of gender-specific hair loss. Genetic predisposition remains paramount, with polygenic inheritance patterns determining individual susceptibility to androgen-mediated follicular damage. Hormonal fluctuations throughout life stages—including pregnancy, menopause, and conditions affecting androgen levels—significantly impact hair loss severity in women. Men face fewer hormonal variables but experience more consistent exposure to high androgen levels throughout adulthood, resulting in predictable progression patterns. Understanding these biological distinctions enables clinicians to develop targeted treatment strategies that address the unique hormonal and genetic factors affecting each gender’s hair loss experience.
Treatment Options Based on Scale Classification
Scale classifications provide essential guidance for selecting appropriate hair loss treatments, allowing clinicians to tailor interventions based on pattern severity and progression stage. Understanding where patients fall on the Ludwig or Norwood scales enables more targeted therapeutic approaches and realistic expectations.
Topical minoxidil remains the first-line treatment for both male and female pattern hair loss across all scale stages. Clinical trials demonstrate that 5% minoxidil solution produces superior hair growth compared to 2% formulations, with approximately 30-40% of users experiencing moderate to dense regrowth[5]. Early-stage patients (Ludwig I or Norwood II-III) often respond particularly well to minoxidil monotherapy.
For more advanced classifications, combination therapy becomes crucial. Oral finasteride, approved for male pattern baldness, effectively halts progression in 80-90% of men with Norwood III-V patterns. Dutasteride, whilst not FDA-approved for hair loss, shows even greater efficacy by inhibiting both types of 5-alpha reductase. Women with Ludwig II-III patterns may benefit from anti-androgen medications alongside minoxidil, though finasteride and dutasteride require careful consideration due to teratogenic risks.
Treatment selection ultimately depends on scale classification severity, with early stages responding to topical treatments alone whilst advanced patterns necessitate comprehensive oral and topical combinations.
Conclusion
Understanding the fundamental differences between the Ludwig Scale vs. Norwood Scale proves invaluable for anyone experiencing hair loss. These classification systems provide essential frameworks for identifying gender-specific patterns, enabling healthcare providers to recommend appropriate hair loss treatments tailored to individual needs. The Ludwig Scale’s focus on central thinning and crown density differs significantly from the Norwood Scale’s emphasis on frontal recession and vertex balding, reflecting the distinct biological mechanisms underlying male and female pattern hair loss.
Early recognition of your position on either scale allows for timely intervention, potentially halting progression and stimulating new hair growth. Modern treatments increasingly target improved blood flow to follicles, addressing a key factor in pattern baldness. Whether utilising topical solutions, oral medications, or advanced therapies, understanding your classification helps determine which approaches will prove most effective for longer-lasting results.
Consulting with qualified healthcare professionals who understand both scales ensures accurate assessment and personalised treatment planning. As research continues advancing our understanding of gender-specific hair loss patterns, these classification systems remain fundamental tools for diagnosis and monitoring treatment progress. By recognising which scale applies to your situation, you can take proactive steps towards maintaining hair health and achieving optimal treatment outcomes.
Frequently Asked Questions
While these scales were designed for specific genders based on typical patterns, some individuals may exhibit atypical hair loss patterns. A healthcare provider can determine which scale is most appropriate for accurate assessment.
Early intervention typically yields better results. Starting treatment at Stage 2-3 on the Norwood Scale or Grade I on the Ludwig Scale often provides the best outcomes, though treatment can be beneficial at any stage.
Common medications like minoxidil may cause scalp irritation, while finasteride can potentially cause side effects including decreased libido, erectile dysfunction, and low libido in some men taking the medication. Always consult a healthcare provider about risks.
While these scales effectively classify current hair loss, they cannot precisely predict individual progression rates. Factors like genetics, stress, overall health, and treatment response all influence how quickly someone may advance through the stages.
References
- Norwood OT. Male pattern baldness: classification and incidence. South Med J. 1975. PMID: 1188424
- Lolli F, Pallotti F, Rossi A, Fortuna MC, Caro G, Lenzi A et al.. Androgenetic alopecia: a review. Endocrine. 2017. PMID: 28349362
- Randall VA. Androgens and hair growth. Dermatol Ther. 2008. PMID: 18844710
- Herskovitz I, Tosti A. Female pattern hair loss. Int J Endocrinol Metab. 2013. PMID: 24719635
- Olsen EA, Weiner MS, Amara IA, DeLong ER. Five-year follow-up of men with androgenetic alopecia treated with topical minoxidil. J Am Acad Dermatol. 1990;22(4):643-646. PMID: 2180995