Introduction
If you’ve ever experienced the sudden surge of heat that characterises hot flushes whilst simultaneously noticing more hair than usual swirling down the shower drain, you’re not alone. These seemingly unrelated symptoms often share a common culprit: your body’s stress response. For many women navigating the menopausal transition, understanding this connection can be the key to finding relief and reclaiming their wellbeing.
The intricate relationship between hot flushes and hair loss extends far beyond simple coincidence. When chronic stress takes hold, it triggers a cascade of hormonal fluctuations that can affect everything from your body’s temperature regulation to the health of your hair follicles. This complex interplay becomes even more pronounced during perimenopause and menopause, when naturally declining hormone levels create additional challenges for your body’s stress management systems.
In this comprehensive guide, we’ll explore the science behind these interconnected symptoms, examining how stress hormones influence both your internal thermostat and hair growth cycles. You’ll discover practical strategies for managing these symptoms through stress reduction techniques, lifestyle modifications, and targeted nutritional approaches. We’ll also discuss when professional medical support might be beneficial and what treatment options are available.
Whether you’re experiencing these symptoms for the first time or have been struggling with them for years, understanding the stress connection empowers you to take control. From evidence-based relaxation techniques to hair-friendly care routines, you’ll find actionable solutions that address the root causes rather than just the symptoms themselves.
Key Takeaways – TL/DR
- Hot flushes and hair shedding are both linked to the body’s stress response system and hormonal changes
- Chronic stress can exacerbate menopausal symptoms including severe hot flushes and telogen effluvium
- Stress management techniques can significantly reduce both hot flash frequency and hair loss
- Understanding the connection helps women develop targeted treatment strategies
- Medical support and lifestyle changes together offer the most effective relief
The Science Behind Hot Flushes and Stress
The connection between hot flushes and stress lies deep within your brain’s thermoregulatory center, where intricate neural pathways orchestrate your body’s temperature control. When stress hormones surge through your system, they disrupt this delicate balance, triggering the vasomotor symptoms that characterise hot flushes whilst activating your sympathetic nervous system in ways that can profoundly impact your overall wellbeing.
Understanding Your Thermoregulatory System
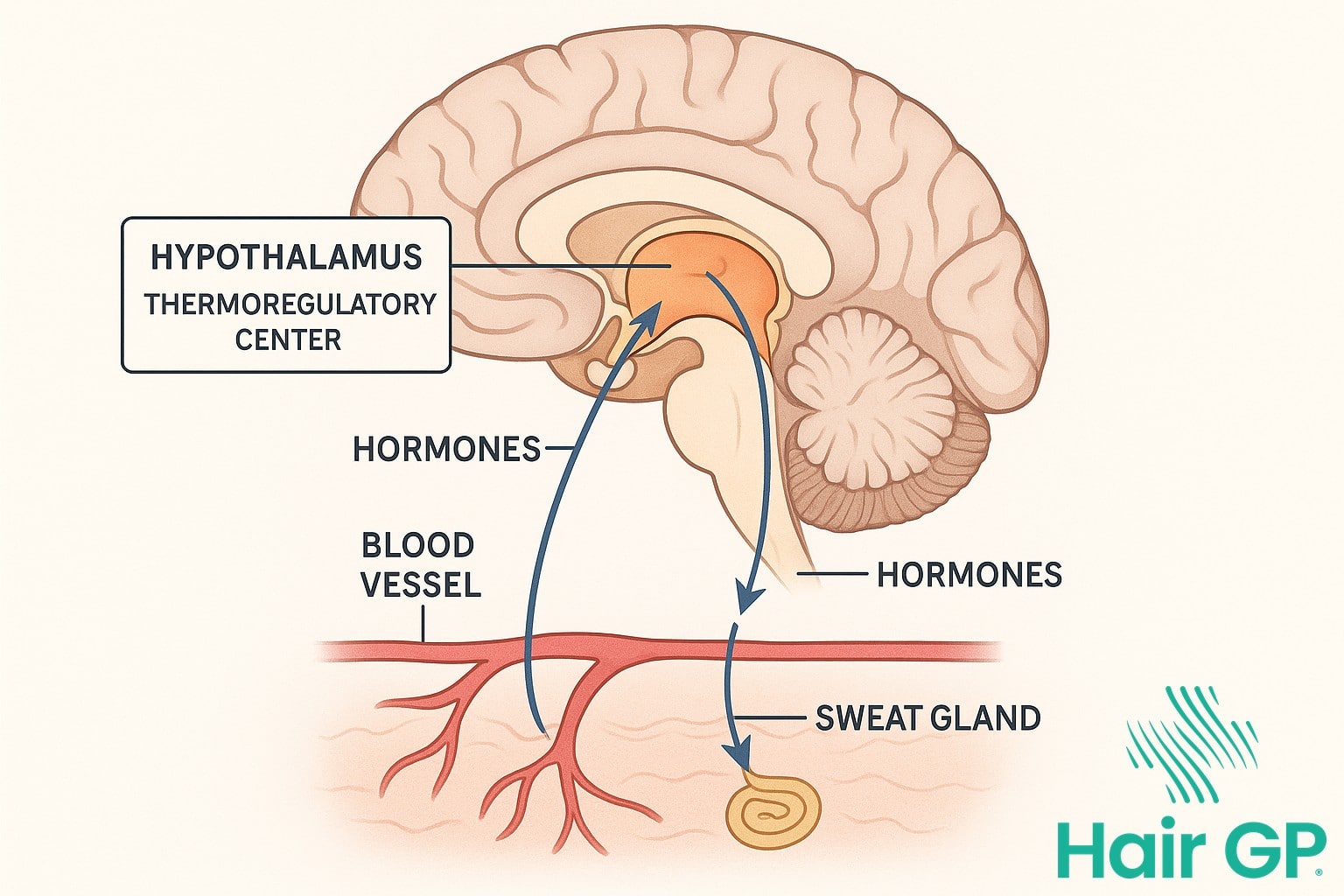
Your hypothalamus, a small but mighty region nestled in your brain, serves as your body’s internal thermostat. This remarkable structure maintains your core temperature within a narrow range by constantly monitoring and adjusting various physiological processes [1]. Under normal circumstances, your hypothalamus responds to temperature changes by triggering appropriate cooling or warming mechanisms—dilating blood vessels near the skin’s surface when you’re too warm, or constricting them when cold.
However, during periods of hormonal fluctuation, particularly when oestrogen levels decline, your temperature set points become unstable. Your hypothalamus essentially receives mixed signals, misinterpreting normal body temperature as excessive heat. This confusion triggers vasomotor symptoms—the sudden dilation of blood vessels that creates the characteristic flush and heat sensation spreading across your chest, neck, and face.
The Role of Stress Hormones
When stress strikes, your body initiates a complex cascade of hormonal responses. Cortisol, your primary stress hormone, plays a particularly crucial role in triggering hot flash episodes. Research demonstrates that elevated cortisol levels directly interfere with temperature regulation by affecting neurotransmitter function in the hypothalamus [2].
Your fight-or-flight response, orchestrated by the sympathetic nervous system, compounds this effect. As adrenaline surges through your bloodstream, it accelerates your heart rate and increases blood pressure, creating the perfect storm for a hot flash episode. This hormone cascade doesn’t operate in isolation—it creates a feedback loop where stress triggers hot flushes, which in turn generate more stress, perpetuating a challenging cycle.
The timing of cortisol release patterns matters significantly. Typically following a circadian rhythm, cortisol peaks in early morning and gradually declines throughout the day. However, chronic stress disrupts these natural patterns, leading to erratic cortisol spikes that can trigger hot flushes at unpredictable moments.
How Stress Triggers Hair Shedding
Chronic stress affects more than just your mental wellbeing—it can directly impact your hair follicles, triggering a condition called telogen effluvium. This stress-induced hair loss occurs when elevated cortisol levels disrupt the normal hair growth cycle, pushing follicles into premature rest phases and causing noticeable shedding.
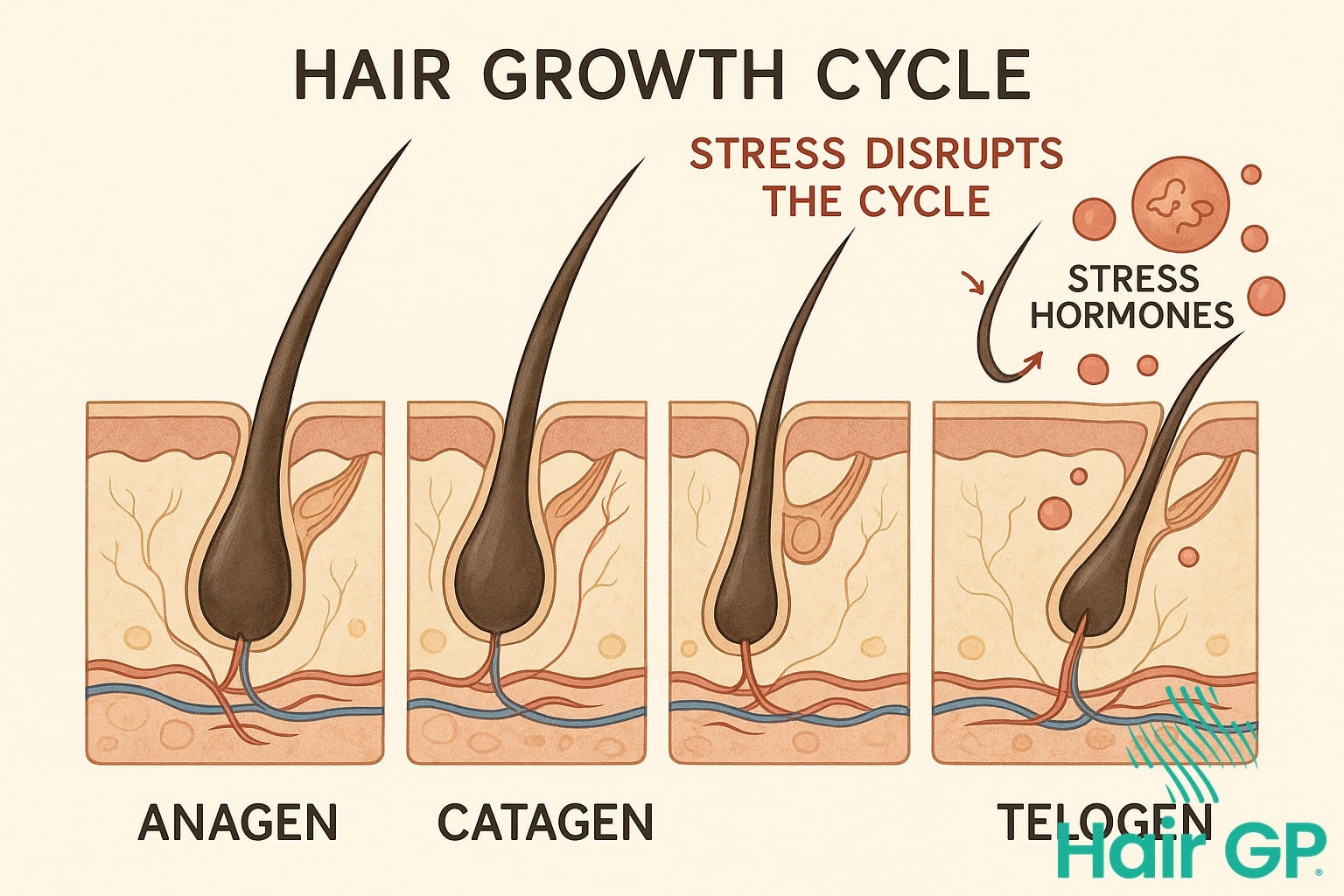
The Hair Growth Cycle Explained
Hair follicles naturally cycle through distinct phases throughout their lifetime. The anagen phase, lasting two to seven years, represents active growth when cells rapidly divide to form new hair strands. Following this, follicles enter a brief transitional period before reaching the telogen phase—a resting state lasting approximately three months. Under normal circumstances, roughly 85-90% of scalp hair remains in the anagen phase, whilst 10-15% rests in telogen [3]. Daily shedding of 50-100 hairs represents healthy follicle turnover as new growth replaces old strands.
Telogen Effluvium and Stress
When chronic stress overwhelms the body, elevated hormone cortisol levels signal hair follicles to prematurely abandon their growth phase. This synchronised shift pushes an abnormally high percentage of follicles—sometimes up to 70%—into telogen simultaneously. The result appears as diffuse hair loss across the scalp, typically becoming noticeable two to three months after the triggering event. Unlike pattern baldness, telogen effluvium affects the entire scalp rather than specific areas. Common triggering events include significant life changes, illness, surgery, or prolonged emotional distress. The interaction between cortisol levels and skin and hair follicles disrupts normal cellular function, temporarily halting growth signals. Fortunately, once stress resolves and cortisol normalises, affected follicles gradually return to their growth phase. Complete recovery typically occurs within six to nine months, with studies showing 95% of cases resolving fully once the underlying stressor is addressed [4].
The Menopause Connection
The menopausal transition marks a profound hormonal shift that creates an environment where both hot flushes and hair loss frequently occur simultaneously. During perimenopause, fluctuating hormone levels not only trigger vasomotor symptoms but also increase follicular sensitivity to stress, establishing a complex relationship between these seemingly disparate symptoms.
Hormonal Changes During Menopause
The journey from premenopausal to postmenopausal status involves dramatic shifts in reproductive hormones. Oestrogen levels begin declining during perimenopause, typically fluctuating unpredictably before dropping to consistently low levels after menopause [5]. This decline affects multiple body systems simultaneously, disrupting temperature regulation whilst altering hair growth cycles. Progesterone levels also decrease significantly, removing its protective effects on both thermoregulation and hair follicles. Meanwhile, relative androgen levels may increase as oestrogen declines, potentially contributing to both vasomotor symptoms and changes in hair distribution patterns. The timing of these hormonal changes varies considerably amongst women, with perimenopausal symptoms potentially lasting several years before complete cessation of menses.
Why Symptoms Intensify Together
The compound effect of hormonal fluctuations and increased stress sensitivity creates a perfect storm for symptom clustering in postmenopausal women. When oestrogen levels drop, the hypothalamic thermostat becomes more sensitive to minor temperature changes, triggering hot flushes more readily [6]. Simultaneously, this hormonal environment increases cortisol reactivity, creating feedback loops that intensify both vasomotor symptoms and stress-related hair shedding. The psychological impact of experiencing multiple symptoms often amplifies stress responses, further exacerbating both conditions. This interconnected relationship explains why many women notice hair loss intensifying during periods of frequent hot flushes, particularly during the early menopausal transition when hormonal fluctuations are most pronounced.

Understanding Your Body’s Stress Response
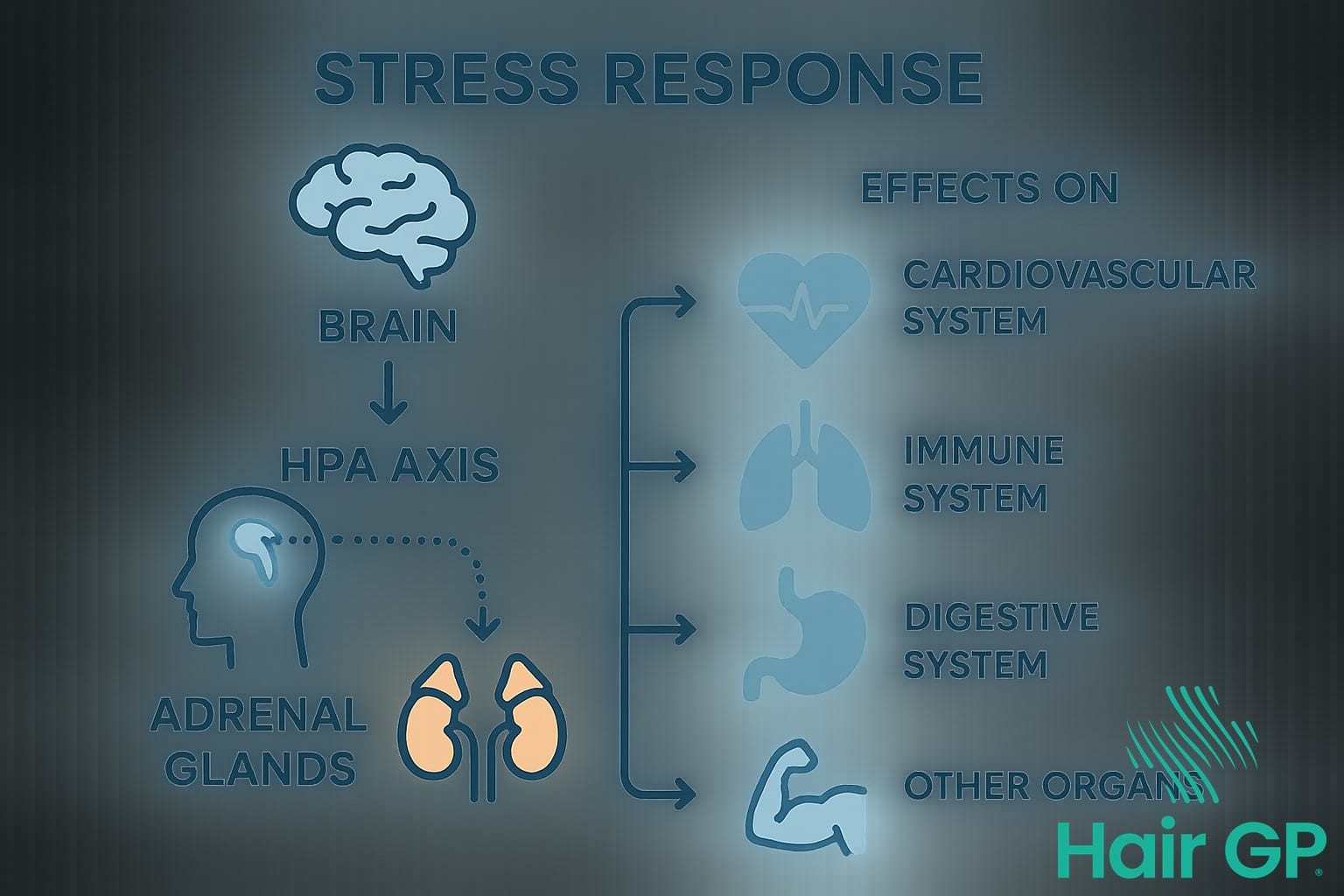
The body’s response to stress involves complex physiological systems working in concert to maintain homeostasis. Understanding these mechanisms helps identify when normal stress responses become harmful, particularly how psychological stressors translate into physical symptoms that affect multiple body systems.
The HPA Axis and Stress
The hypothalamic-pituitary-adrenal (HPA) axis orchestrates the body’s primary stress response through a sophisticated hormone cascade [7]. When encountering stressful life events, the hypothalamus releases corticotropin-releasing hormone (CRH), stimulating the pituitary gland to produce adrenocorticotropic hormone (ACTH). This prompts the adrenal glands to release cortisol and other stress hormones. Under normal circumstances, negative feedback mechanisms maintain balance, with elevated cortisol signalling the hypothalamus to reduce CRH production. However, chronic stress disrupts these regulatory processes, leading to HPA axis dysregulation characterised by altered cortisol rhythms, heightened stress sensitivity, and impaired recovery from acute stressors.
Recognising Chronic Stress Patterns
Distinguishing between normal stress levels and harmful chronic patterns requires awareness of multiple indicators [8]. Physical symptoms include persistent fatigue, unexplained pain, digestive issues, and frequent infections due to compromised immunity. Emotional signs encompass anxiety, irritability, depression, and increased vulnerability to panic attack episodes. Behavioural changes often manifest as sleep disturbances, appetite alterations, social withdrawal, and reliance on unhealthy coping mechanisms. Recognising these patterns early enables intervention before stress-related damage becomes entrenched, highlighting the importance of monitoring both physical and psychological responses to life’s challenges.
Managing Hot Flushes Through Stress Reduction
Effective stress management significantly reduces both the frequency and intensity of hot flushes during menopause. Research demonstrates that women who practice structured stress reduction techniques experience up to 40% fewer hot flushes compared to those using conventional approaches alone [9]. By calming the nervous system and regulating hormonal fluctuations, these evidence-based methods offer relief for treating hot flushes whilst improving overall well being.
Mindfulness and Breathing Techniques
Specific practices that directly calm the autonomic nervous system prove particularly effective for managing severe hot flushes. Paced breathing, involving slow, deep breaths at 6-8 cycles per minute, reduces hot flash severity by 50% when practised twice daily [10]. Body scan meditation helps identify tension patterns that trigger episodes, whilst progressive muscle relaxation counteracts the stress response that intensifies symptoms. Women who dedicate just 15 minutes daily to these techniques report fewer night sweats and improved emotional regulation. The key lies in consistency—regular practice strengthens the body’s relaxation response, creating lasting physiological changes that reduce hot flash triggers.
Lifestyle Modifications That Work
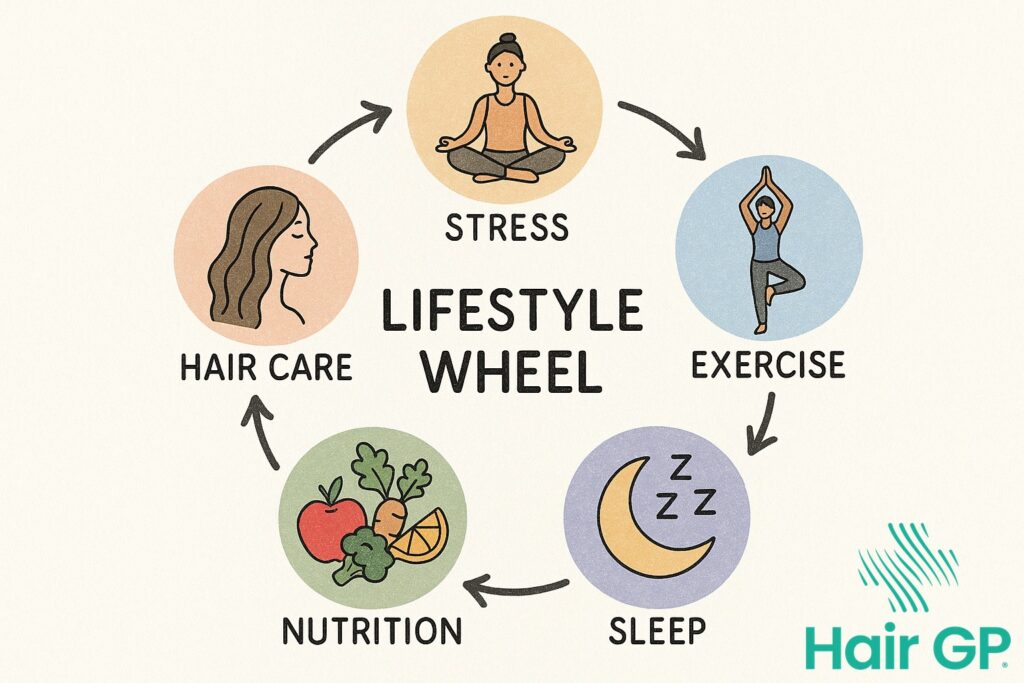
Daily lifestyle changes complement mindfulness practices in reducing stress-related hot flushes. Regular moderate exercise, particularly yoga or walking for 30 minutes daily, decreases hot flash frequency by 35% whilst improving mood swings [11]. Establishing consistent sleep hygiene—including cool bedroom temperatures and regular bedtimes—minimises night sweats disruption. Dietary adjustments matter too: reducing caffeine and alcohol intake whilst increasing phytoestrogen-rich foods like soya helps stabilise hormonal fluctuations. These modifications work synergistically, creating an environment where the body can better manage temperature regulation whilst supporting emotional well being throughout the menopausal transition.

Hair Health During Hormonal Changes
Supporting hair health during hormonal changes requires a gentle, comprehensive approach that addresses both internal and external factors. For midlife women experiencing hormonal fluctuations, nourishing hair follicles from within becomes essential. A diet rich in protein, iron, B-vitamins, and omega-3 fatty acids provides the building blocks needed for healthy hair growth. Incorporating foods like salmon, eggs, leafy greens, and nuts can help counteract the effects of declining hormones on hair structure.
Gentle hair care practices become particularly important during this transition. Avoiding excessive heat styling, reducing washing frequency to preserve natural oils, and using sulphate-free shampoos can minimise additional stress on vulnerable hair follicles. Scalp massage with lightweight oils like rosemary or jojoba can improve circulation whilst providing a calming ritual during stressful periods.
Whilst some hair changes are normal during hormonal transitions, certain signs warrant professional attention. If hair loss continues for more than six months after a stressful event, appears in patches, or is accompanied by scalp irritation, consulting a healthcare provider is advisable. They can assess whether underlying conditions beyond natural hormonal changes might be contributing to hair loss. Early intervention often yields better outcomes, particularly when addressing the complex interplay between stress, hormones, and hair health in midlife women.

Treatment Options and Medical Support
Medical interventions offer significant relief for women experiencing hot flushes and stress-related hair loss during menopause. Healthcare providers can prescribe various treatments ranging from hormone replacement therapy to non-hormonal alternatives, with selection based on individual health profiles and symptom severity. Understanding available options enables informed decision-making about managing menopausal symptoms effectively.
Hormone Replacement Therapy Options
Hormone replacement therapy remains the most effective treatment for vasomotor symptoms, reducing hot flash frequency by up to 75% [12]. Available HRT types include oestrogen-only therapy for women without a uterus and combined oestrogen-progesterone formulations for those with intact uterus (ie. who havent undergone a hysterectomy). Recent medical news highlights improved safety profiles when therapy is initiated within ten years of menopause onset [13].
Candidacy assessment considers age, cardiovascular health, and personal cancer history. Benefits extend beyond body temperature regulation to include bone protection and potential mood improvement, helping menopause elevate quality of life rather than diminish it.
Non-Hormonal Medical Treatments
For women unable or unwilling to use HRT, several non-hormonal options provide meaningful symptom relief. Selective serotonin reuptake inhibitors reduce hot flash severity by approximately 50% whilst simultaneously addressing anxiety symptoms . Gabapentin offers an alternative mechanism, particularly effective for night-time vasomotor symptoms.
Topical treatments including vaginal moisturisers and lubricants address localised symptoms without systemic effects. Healthcare consultation becomes essential when symptoms significantly impact daily functioning or when over-the-counter remedies prove insufficient.
Lifestyle Strategies for Better Well-being
A holistic approach to well being during the menopause transition addresses both hot flushes and hair health through interconnected lifestyle strategies. Rather than treating symptoms in isolation, integrated modifications create synergistic benefits that support overall health whilst managing specific concerns. This comprehensive approach proves particularly effective for perimenopausal and postmenopausal women seeking sustainable relief.
Nutrition forms the foundation of symptom management, with anti-inflammatory foods reducing hot flash frequency whilst providing essential nutrients for hair growth. Omega-3 rich foods, leafy greens, and adequate protein support hormonal balance and follicle health simultaneously. Regular meal timing stabilises blood sugar levels, preventing the metabolic fluctuations that trigger temperature dysregulation.
Physical activity enhances circulation to both skin and scalp whilst moderating hormonal fluctuations. Low-impact exercises like swimming and yoga prove especially beneficial, avoiding excessive heat generation whilst maintaining cardiovascular health. Even premenopausal women benefit from establishing these routines early, creating protective habits before symptoms intensify.
Quality sleep and effective stress management techniques work synergistically to reduce common stressors that exacerbate both conditions. Establishing consistent sleep schedules helps regulate body temperature whilst supporting cellular repair processes essential for hair growth. Mindfulness practices and breathing exercises provide immediate relief from acute symptoms whilst building long-term resilience against the physiological changes of menopause, creating sustainable improvements in overall health and symptom management.

Conclusion
Understanding the intricate relationship between hot flushes, hair shedding, and the stress response provides crucial insight for managing menopausal symptoms effectively. This interconnected web of physiological changes demonstrates how chronic stress amplifies both vasomotor symptoms and follicular disruption, creating a challenging cycle that impacts overall well being.
The evidence clearly shows that addressing these symptoms in isolation often yields limited results. Instead, a comprehensive approach that acknowledges their shared hormonal and neurological pathways offers the most promising outcomes. By implementing targeted stress management techniques alongside conventional treatments, women can significantly reduce symptom severity whilst improving their quality of life.
Taking control of your stress response through mindfulness, regular exercise, and therapeutic interventions not only diminishes hot flushes but also supports healthier hair growth patterns. This holistic strategy recognises that menopausal symptoms don’t exist in separate compartments but rather influence each other through complex biological mechanisms.
Moving forward with this integrated understanding empowers women to make informed decisions about their health. Rather than feeling overwhelmed by multiple symptoms, recognising their common roots in stress and hormonal fluctuations provides a clear path towards comprehensive symptom relief and enhanced well being during this transitional phase.
Frequently Asked Questions
Yes, stress can trigger hot flush-like symptoms even in premenopausal women through activation of the sympathetic nervous system and stress hormone release. However, these are typically less frequent and severe than menopausal hot flushes.
Telogen effluvium from stress usually resolves within 3-6 months after the stressor is removed or managed. Hair regrowth typically begins 2-3 months after shedding stops, with full recovery taking 6-12 months.
Hot flushes typically decrease over time, usually improving significantly within 2-5 years post-menopause. Hair changes may be partially permanent due to hormonal shifts, but stress-related shedding is usually temporary with proper management.
Hot flushes involve sudden warmth, sweating, and flushing lasting 1-5 minutes, while panic attacks include intense fear, rapid heartbeat, and breathing difficulties lasting 5-20 minutes. Both can be triggered by stress but have different underlying mechanisms.
Consult a healthcare provider if hot flushes severely impact daily life, occur more than 7 times daily, or if hair loss is sudden, patchy, or accompanied by other symptoms like fatigue or weight changes.
References
- Romanovsky AA. Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am J Physiol Regul Integr Comp Physiol. 2007. PMID: 17008453
- Thurston RC, Maki PM, Derby CA, Sejdić E, Aizenstein HJ. Menopausal hot flashes and the default mode network. Fertil Steril. 2015. PMID: 25910572
- Malkud S. Telogen Effluvium: A Review. J Clin Diagn Res. 2015. PMID: 26500992
- Asghar F, Shamim N, Farooque U, Sheikh H, Aqeel R. Telogen Effluvium: A Review of the Literature. Cureus. 2020. PMID: 32607303
- El Khoudary SR, Greendale G, Crawford SL, Avis NE, Brooks MM, Thurston RC et al.. The menopause transition and women's health at midlife: a progress report from the Study of Women's Health Across the Nation (SWAN). Menopause. 2019. PMID: 31568098
- Thurston RC. Vasomotor symptoms: natural history, physiology, and links with cardiovascular health. Climacteric. 2018. PMID: 29390899
- Spencer RL, Deak T. A users guide to HPA axis research. Physiol Behav. 2017. PMID: 27871862
- McEwen BS, Akil H. Revisiting the Stress Concept: Implications for Affective Disorders. J Neurosci. 2020. PMID: 31896560
- Goldstein KM, Shepherd-Banigan M, Coeytaux RR, McDuffie JR, Adam S, Befus D et al.. Use of mindfulness, meditation and relaxation to treat vasomotor symptoms. Climacteric. 2017. PMID: 28286985
- Cramer H, Peng W, Lauche R. Yoga for menopausal symptoms-A systematic review and meta-analysis. Maturitas. 2018. PMID: 29452777
- Daley AJ, Thomas A, Roalfe AK, Stokes-Lampard H, Coleman S, Rees M et al.. The effectiveness of exercise as treatment for vasomotor menopausal symptoms: randomised controlled trial. BJOG. 2015. PMID: 25516405
- Crandall CJ, Mehta JM, Manson JE. Management of Menopausal Symptoms: A Review. JAMA. 2023. PMID: 36749328
- Nappi RE. The 2022 hormone therapy position statement of The North American Menopause Society: no news is good news. Lancet Diabetes Endocrinol. 2022. PMID: 36270315