Introduction
If you’ve noticed excessive hair shedding weeks or months after recovering from COVID-19, you’re not alone. Studies indicate that up to 25% of COVID survivors experience significant hair loss, making it one of the most common yet least discussed aspects of post COVID syndrome. This widespread phenomenon has left millions searching for answers about why their hair is falling out and whether it will grow back.
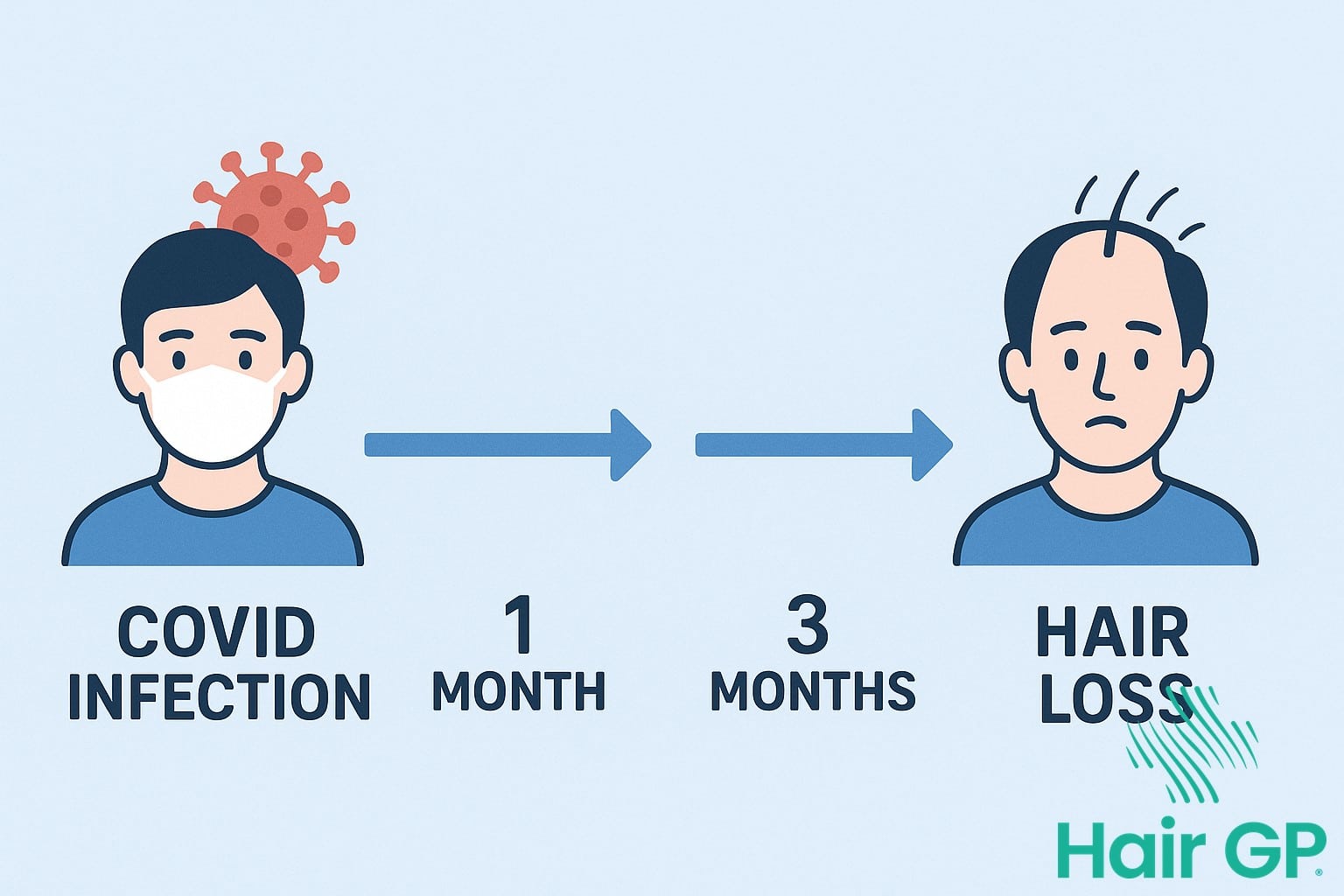
The primary culprit behind this distressing symptom is telogen effluvium, a temporary condition where physical or emotional stress forces hair follicles into a resting phase, leading to dramatic shedding approximately 2-3 months after the triggering event. For many, the connection between hair loss and long COVID comes as a surprise, particularly when other symptoms have resolved.
This comprehensive guide explores the medical mechanisms linking COVID-19 to hair loss, distinguishes between normal shedding and concerning patterns, and examines why some patients experience prolonged symptoms whilst others recover quickly. We’ll also address the emotional impact, identify high-risk groups, review current research, and most importantly, provide clear recovery timelines and evidence-based strategies to support hair regrowth.
Key Takeaways – TL/DR
- Up to 25% of COVID-19 survivors experience significant hair loss 2-3 months after infection
- Telogen effluvium is the primary mechanism, pushing 30-50% of hair follicles into premature shedding phase
- Most cases resolve within 6-9 months without treatment, though recovery varies by individual
- Nutritional support with iron, zinc, and vitamin D can accelerate hair regrowth by up to 30%
Understanding Hair Loss and Long COVID: The Lingering Effects Nobody Talks About
The global pandemic caused by SARS-CoV-2 has revealed numerous lingering effects that extend far beyond the acute infection phase. Amongst these prolonged symptoms, hair loss represents one of the most common manifestations of post COVID syndrome, yet it remains significantly under-reported in mainstream medical discussions. A systematic review published in 2022 found that hair loss affected between 20-25% of COVID-19 survivors, making it more prevalent than many widely recognised symptoms [1].
Despite affecting millions worldwide, post COVID-19 hair loss rarely features in public health messaging or recovery guidance. This oversight stems partly from its delayed onset—typically occurring 2-3 months after infection—and the misconception that it’s merely cosmetic rather than a genuine medical concern. Research indicates that the inflammatory cascade triggered by SARS-CoV-2 disrupts normal hair follicle cycling, pushing actively growing hairs prematurely into the resting phase [2].
The psychological impact of this symptom compounds the challenges of post COVID syndrome recovery. Patients already grappling with fatigue, brain fog, and other prolonged symptoms find themselves confronting visible changes that affect their self-image and confidence. Understanding this connection helps validate patient experiences and guides appropriate treatment approaches, particularly as evidence suggests most cases resolve within 6-9 months with proper support.
Common Symptoms: When COVID-19 Affects Your Hair
COVID-related hair loss presents with distinct patterns that differ from typical hair thinning conditions. Beyond the more familiar unusual symptoms like persistent cough or loss of taste, many COVID survivors notice hair loss manifesting as sudden, dramatic shedding that affects the entire scalp rather than isolated patches.
Recognizing Excessive Hair Shedding Patterns
The hallmark of post-COVID excessive hair loss is diffuse hair loss across the scalp, with patients reporting finding large clumps on their pillow, in the shower, or whilst brushing. Daily hair fall typically exceeds 100-150 strands—significantly more than the normal 50-100. You might notice visible scalp areas, particularly around the crown and temples, whilst shower drains become clogged with unprecedented amounts of hair.
Additional symptoms often accompany the shedding, including an itchy scalp, tenderness, or burning sensations. Unlike pattern baldness, this hair thinning affects the entire head uniformly. Most patients first notice hair loss approximately 2-3 months after their COVID infection, coinciding with when other long-COVID symptoms may persist or emerge.
Hair Shedding vs. Normal Hair Loss: Understanding the Difference
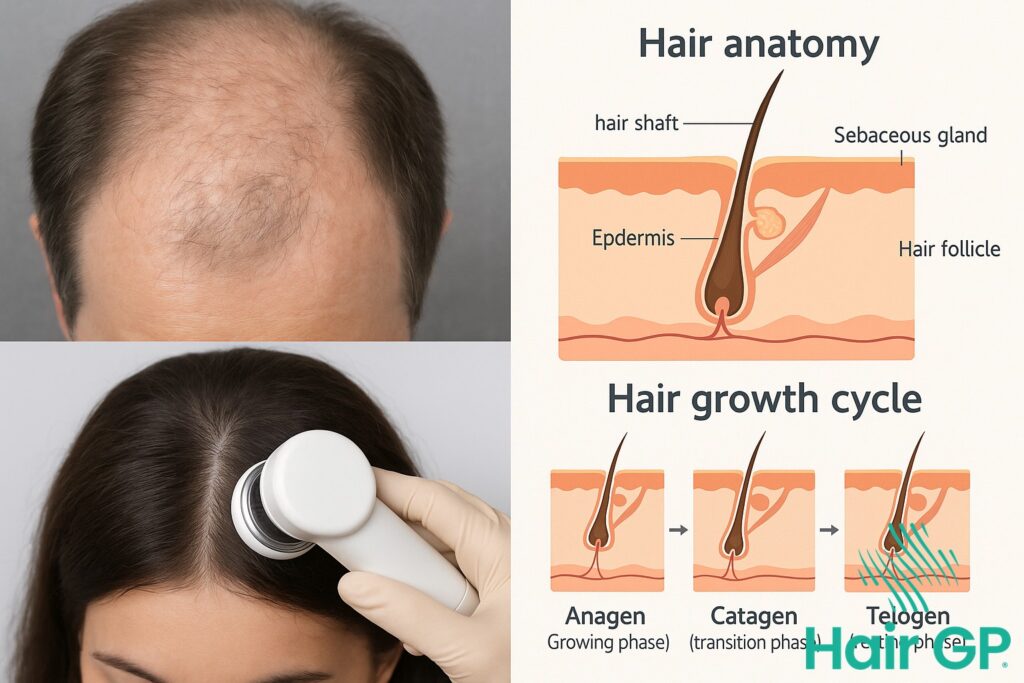
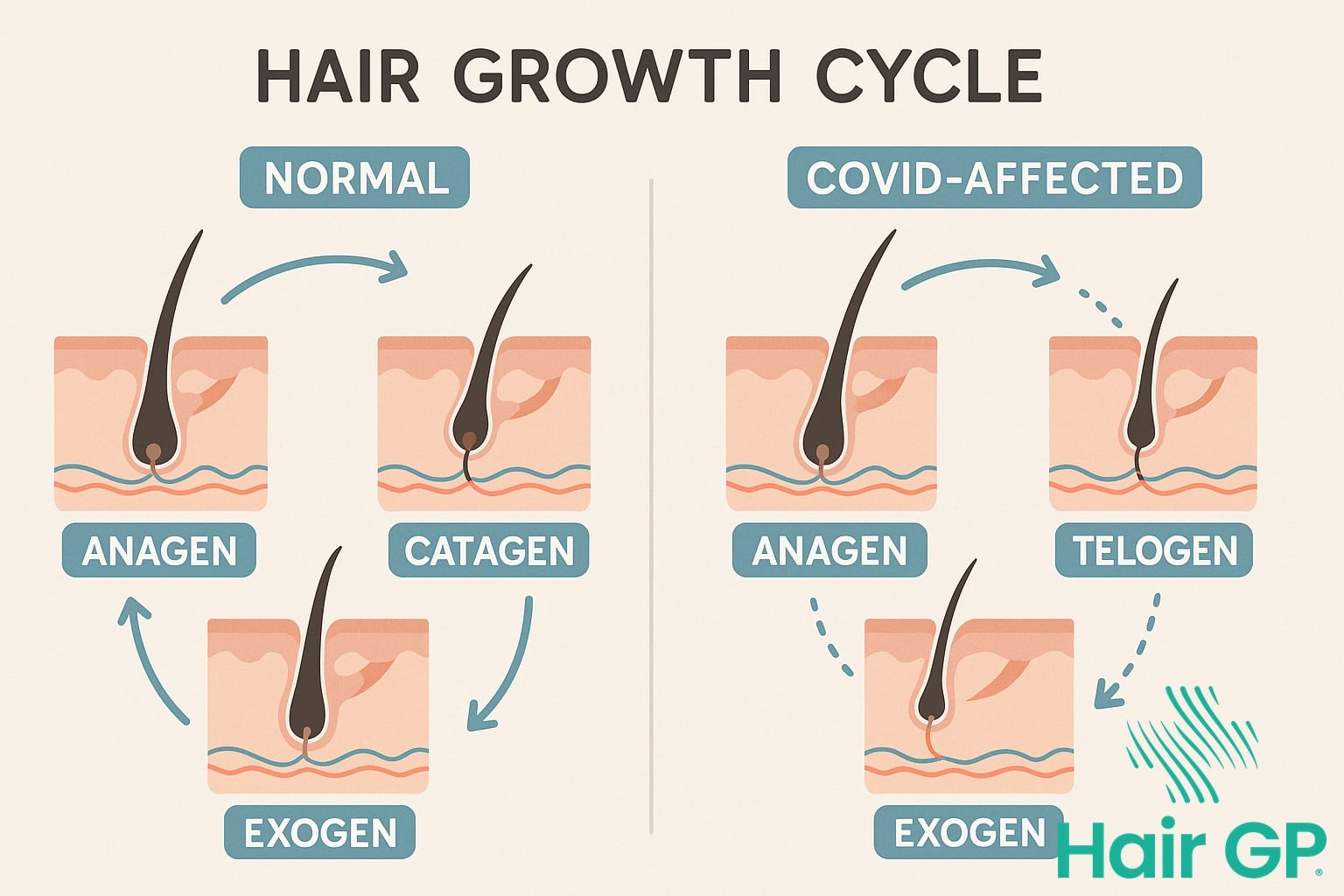
Understanding whether your hair loss is COVID-related or part of normal shedding cycles is crucial for determining next steps. Typically, we lose between 50-100 hairs daily as part of the natural hair growth cycle, with follicles cycling through growing phase (anagen phase), transition, and resting phase independently [3]. This gradual shedding maintains overall hair density whilst allowing for continuous renewal.
COVID-induced telogen effluvium dramatically disrupts this balance, pushing up to 50% of follicles simultaneously into the telogen phase. Unlike normal shedding, you’ll notice clumps of hair coming out during washing or brushing, with visible thinning occurring within weeks. The telogen phase typically lasts 2-3 months before new hair begins pushing out the old [4]. Whilst alarming, this temporary hair loss follows a predictable timeline: excessive shedding phase peaks around three months post-infection, then gradually improves as follicles re-enter their growth phase. Most importantly, this condition resolves completely once follicles resume their normal cycling pattern.
COVID-19 and Telogen Effluvium: The Medical Connection
COVID-19 triggers telogen effluvium through a complex cascade of inflammatory and stress responses that disrupt the normal hair growth cycle. The virus induces systemic inflammation, characterised by elevated cytokine levels and prolonged immune system activation, which collectively signal hair follicles to enter premature resting phase [5]. This biological stress response typically manifests as widespread hair shedding approximately 2-3 months following the initial triggering event.
Acute vs. Chronic Telogen Effluvium After COVID
Most post-COVID telogen effluvium hair loss presents as acute telogen effluvium, resolving within 3-6 months as follicles naturally resume their growth cycle [6]. However, approximately 10-20% of patients develop chronic telogen effluvium extending beyond six months, particularly those experiencing prolonged physical stress from long COVID symptoms. Recovery predictors include baseline health status, severity of initial infection, and presence of persistent inflammation. Patients with high fever during acute infection show increased risk of developing more severe hair loss patterns. The distinction between acute and chronic forms proves crucial for treatment planning, as chronic cases may require targeted interventions addressing underlying inflammatory markers. This stressful event often compounds existing health anxieties, potentially perpetuating the shedding cycle through sustained cortisol elevation.
Long COVID and Persistent Hair Loss Patterns
Long COVID patients frequently experience persistent hair loss that extends well beyond typical telogen effluvium recovery periods, with studies indicating that approximately 22% of individuals with post COVID syndrome report ongoing alopecia six months after initial infection [7]. These lingering effects correlate strongly with other prolonged symptoms including chronic fatigue syndrome, persistent cough, and cognitive dysfunction, suggesting systemic inflammatory mechanisms at play.
The persistent nature of hair loss in long COVID appears linked to sustained inflammatory markers and dysregulated immune responses that characterise the condition [8]. Patients experiencing concurrent post traumatic stress disorder from their COVID experience show particularly protracted recovery patterns, as psychological stress compounds the physiological disruption to hair follicle cycling. This creates a complex therapeutic challenge where addressing both the underlying inflammation and stress response becomes essential for restoration.
Brain Fog and Hair Loss: Connected Symptoms of Long COVID
The neurological manifestations of long COVID, particularly brain fog, share underlying inflammatory pathways with physical symptoms like hair loss. Research suggests neuroinflammation triggers both cognitive dysfunction and disrupts hair follicle cycles through systemic inflammatory cascades. Patients experiencing persistent fatigue, dizziness, and cognitive impairment often report concurrent hair shedding, indicating interconnected pathophysiological mechanisms.
Autonomic dysfunction links these diverse symptoms—from anosmia and altered taste and smell to vertigo and exhaustion. The same inflammatory processes affecting neural pathways can disrupt blood flow to hair follicles. Additionally, conditions like myocarditis and chronic insomnia create metabolic stress that compounds follicular damage. This multi-system involvement explains why patients with neurological long COVID symptoms frequently develop telogen effluvium, highlighting the importance of comprehensive treatment approaches addressing both cognitive and physical manifestations.
Emotional Stress and Post-COVID Hair Loss
The pandemic’s psychological toll significantly amplifies hair loss beyond the virus’s direct physical effects. Emotional stress from isolation, uncertainty, and loss creates a dual burden on hair follicles, where anxiety and depression compound the biological stress caused by COVID infection itself.
Managing Pandemic-Related Anxiety for Hair Health
Chronic emotional stress triggers cortisol release, further disrupting hair growth cycles already affected by illness. Post traumatic stress disorder (PTSD), grief from bereavement, and pandemic-related panic have all contributed to widespread telogen effluvium cases. Breaking this stress cycle proves essential for recovery. Regular meditation reduces cortisol levels whilst improving sleep quality—both crucial for hair regeneration. Maintaining consistent sleep hygiene helps regulate hormonal balance, whilst moderate exercise releases endorphins that counter anxiety and depression. These coping strategies support both mental wellbeing and physical health, creating optimal conditions for hair regrowth as you recover from COVID’s multifaceted impact.
Alopecia Areata vs. COVID-Related Hair Loss
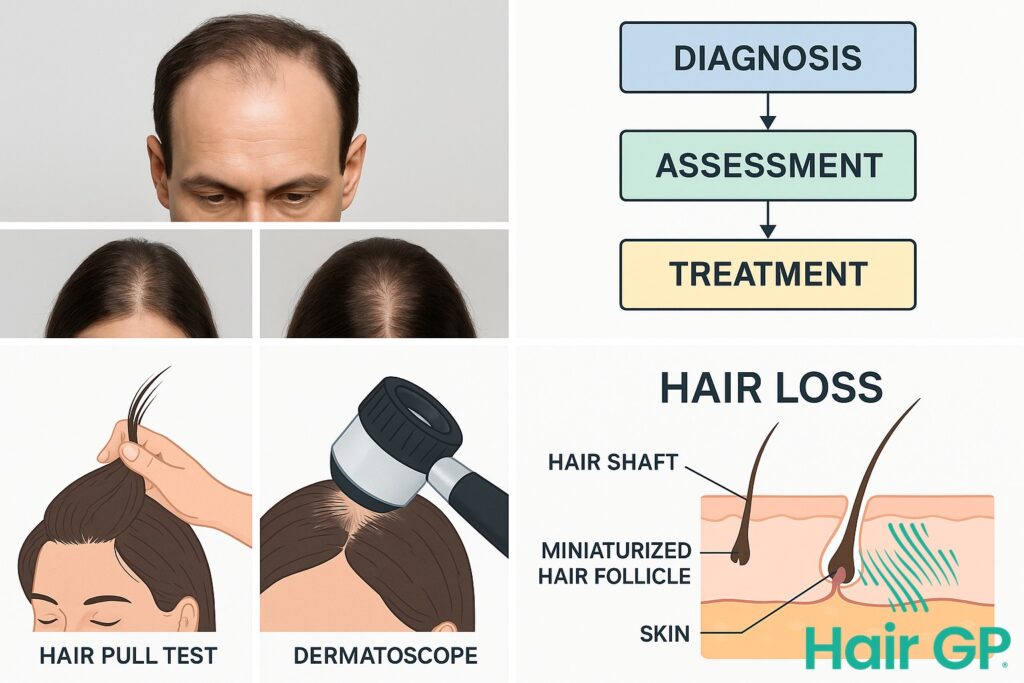
Distinguishing between alopecia areata and COVID-related telogen effluvium requires understanding their fundamental differences. Alopecia areata presents as distinct small patches of complete hair loss with smooth, coin-sized bald spots, caused by autoimmune attack on hair follicles [9]. In contrast, COVID-induced telogen effluvium manifests as diffuse hair loss throughout the scalp, creating overall thinning rather than discrete patches [5]. While alopecia may become permanent without treatment, COVID-related shedding represents temporary hair disruption typically resolving within 6-9 months. Other types of hair loss, including androgenetic alopecia, require different diagnostic approaches. Specialist assessment becomes crucial when patches expand rapidly, affect eyebrows or body hair, or persist beyond expected recovery timeframes [10].

Disease Severity and Hair Loss Risk Factors
Disease severity emerges as the primary predictor of telogen effluvium development post-infection. Patients hospitalised with severe COVID-19 demonstrate significantly higher hair loss incidence, with studies reporting 48% prevalence amongst ICU survivors versus 27% in general ward patients [5]. Risk factors compound exponentially when pneumonia complications require mechanical ventilation, with mean age above 50 showing doubled vulnerability. Hospital discharge protocols now incorporate hair loss screening, recognising the correlation between hospitalization duration and follicular disruption severity.
Pre-existing metabolic conditions amplify risk profiles substantially. Diabetic patients in hospitals experience 1.7-fold increased telogen effluvium rates compared to non-diabetic cohorts [6]. Gender disparities prove striking, with women demonstrating 2.3 times higher susceptibility despite comparable disease severity markers. ICU admission correlates with delayed-onset presentations, typically manifesting 3-4 months post-discharge rather than the standard 6-12 week timeline. These severity-dependent patterns guide risk stratification protocols, enabling targeted preventive interventions for high-risk populations during acute care phases.
Higher Risk Groups for Post-COVID Hair Loss
Certain populations demonstrate increased vulnerability to post-COVID hair loss, with women experiencing disproportionately higher rates compared to male counterparts [11]. This gender disparity reflects both hormonal influences on women’s hair health and differential immune responses between sexes. Female patients report telogen effluvium at twice the frequency of males following COVID-19 infection.
Age significantly impacts recovery trajectories, with older adults facing prolonged shedding phases due to age-related hair changes and slower follicle regeneration [12]. Nutritional deficiencies, particularly iron, vitamin D, and zinc insufficiencies, compound vulnerability across all demographics, creating synergistic effects that intensify post-viral hair loss severity.
Data Collection and Research on COVID Hair Loss
International research teams have conducted extensive investigations into COVID-related hair loss through multiple methodological approaches. A comprehensive systematic review and meta analysis examining 25 studies with combined sample size exceeding 48,000 patients revealed telogen effluvium prevalence ranging from 24-67% post-infection [5]. One pivotal cross sectional study that study aimed to quantify hair loss severity study reported median onset at 58 days following initial infection, with recovery typically occurring within 3-6 months [6]. Statistical analysis of multicenter data demonstrated significant correlations between disease severity and subsequent hair loss intensity. Additionally, numerous case reports have documented atypical presentations, including alopecia areata and anagen effluvium, providing crucial insights into diverse pathophysiological mechanisms underlying COVID-associated hair disorders.
Hair Loss After COVID: Timeline and Recovery Expectations
Understanding the timeline from COVID infection to hair regrowth helps set realistic expectations for recovery. Most patients notice hair shedding two to three months after infection, with recovery beginning several months later as the body heals and follicles reactivate.
When to Expect More Hair Growth
Initial hair regrowth typically becomes visible after three months from when shedding peaks, though individual timelines vary considerably. During the first few months of recovery, new hair grows as fine, delicate strands that gradually strengthen over time. Visible improvement usually occurs within three to six months, with more hair density becoming apparent as follicles synchronise their growth cycles. Complete recovery often requires patience—whilst some individuals regrow their full hair density within six months, others may need up to twelve months for complete restoration. Recovery tracking through monthly photographs helps monitor progress, as gradual changes prove difficult to perceive daily. Most importantly, consistent regrowth indicates healthy follicle function, even when the process feels frustratingly slow.

Conclusion
COVID-related telogen effluvium typically resolves within six to nine months, with complete hair regrowth occurring in most patients without intervention. Whilst hair loss and long COVID symptoms can feel distressing, understanding the temporary nature of this condition provides reassurance during recovery.
Supporting your body’s natural healing requires patience alongside targeted strategies. Maintain optimal nutrition with iron, vitamin D, and B-complex supplements, practise stress-reduction techniques, and establish gentle hair care routines. These foundational approaches enhance recovery whilst your hair follicles naturally return to their growth phase.
Schedule a consultation with a hair loss specialist if shedding persists beyond six months or worsens despite self-care measures. Professional assessment can identify whether additional treatment options are needed or if underlying conditions require attention. Specialists can provide personalised guidance, monitoring progress through trichoscopy and recommending evidence-based interventions when necessary.
Remember that recovery remains the norm, not the exception. Your hair follicles retain their ability to regenerate, and with appropriate support, full restoration typically occurs.
Frequently Asked Questions
Most COVID-related hair loss resolves within 6-9 months. Acute telogen effluvium typically begins 2-3 months after infection and gradually improves. However, some long COVID patients may experience extended shedding requiring medical intervention.
COVID-related hair loss is typically temporary. The telogen effluvium triggered by COVID affects the hair growth cycle but doesn’t damage follicles permanently. Over 90% of patients experience full recovery, though the timeline varies.
Iron, zinc and vitamin D can support recovery from COVID-related hair loss. However, consult a healthcare provider before starting supplements, as excessive amounts can be harmful. A balanced diet often provides adequate nutrients.
See a board certified dermatologist if hair loss persists beyond 6 months, worsens progressively, or includes other symptoms like scalp pain or inflammation. Early intervention can identify underlying issues and accelerate recovery.
Women report COVID-related hair loss more frequently than men, possibly due to hormonal factors and longer hair making shedding more noticeable. However, both genders experience similar telogen effluvium mechanisms and recovery timelines.
References
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A et al.. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021. PMID: 34373540
- Moreno-Arrones OM, Lobato-Berezo A, Gomez-Zubiaur A, Arias-Santiago S, Saceda-Corralo D, Bernardez-Guerra C et al.. SARS-CoV-2-induced telogen effluvium: a multicentric study. J Eur Acad Dermatol Venereol. 2021. PMID: 33220124
- Trüeb RM. Systematic approach to hair loss in women. J Dtsch Dermatol Ges. 2010. PMID: 20105246
- Malkud S. Telogen Effluvium: A Review. J Clin Diagn Res. 2015. PMID: 26500992
- Nguyen B, Tosti A. Alopecia in patients with COVID-19: A systematic review and meta-analysis. JAAD Int. 2022. PMID: 35224518
- Abou-Rahal J, Abdullah L, Kurban M, Abbas O. Letter to the editor regarding the article ''Rossi A, Magri F, Michelini S, et al. New onset of alopecia areata in a patient with SARS-COV-2 infection: Possible pathogenetic correlations? J Cosmet Dermatol. 2021 Mar 19. doi: 10.1111/jocd.14080". J Cosmet Dermatol. 2021. PMID: 33853206
- Davis HE, McCorkell L, Vogel JM, Topol EJ. Author Correction: Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023. PMID: 37069455
- Altmann DM, Whettlock EM, Liu S, Arachchillage DJ, Boyton RJ. Author Correction: The immunology of long COVID. Nat Rev Immunol. 2023. PMID: 37723341
- Strazzulla LC, Wang EHC, Avila L, Lo Sicco K, Brinster N, Christiano AM et al.. Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018. PMID: 29241771
- Sharquie KE, Jabbar RI. COVID-19 infection is a major cause of acute telogen effluvium. Ir J Med Sci. 2022. PMID: 34467470
- Farrar JE, Trujillo TC, Mueller SW, Beltran L, Nguyen C, Hassell K et al.. Evaluation of a patient specific, targeted-intensity pharmacologic thromboprophylaxis protocol in hospitalized patients with COVID-19. J Thromb Thrombolysis. 2022. PMID: 34410561
- Olds H, Liu J, Luk K, Lim HW, Ozog D, Rambhatla PV. Telogen effluvium associated with COVID-19 infection. Dermatol Ther. 2021. PMID: 33405302