Introduction
Hair loss affects millions of women worldwide, creating both physical and emotional challenges that can significantly impact quality of life. Among the various causes of hair loss in women, female pattern hair loss and telogen effluvium stand out as the two most prevalent conditions, each affecting countless individuals seeking answers and effective treatment options.
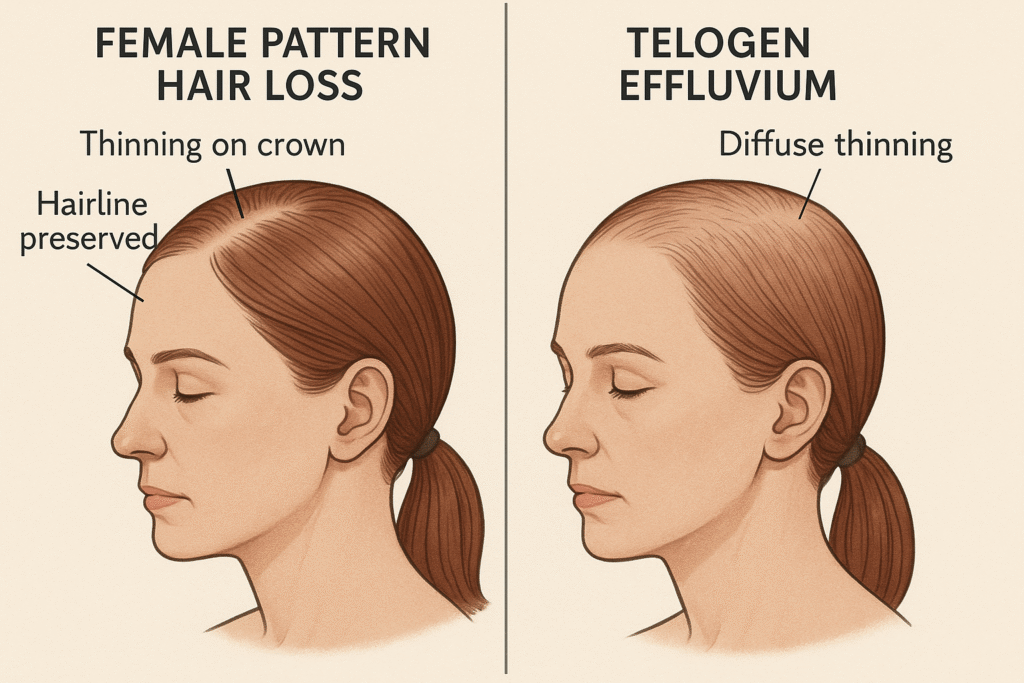
While both female pattern hair loss and telogen effluvium result in noticeable hair thinning, these conditions have distinctly different characteristics, underlying causes, and treatment approaches. Female pattern hair loss, also known as androgenetic alopecia, typically develops gradually over time due to genetic and hormonal factors. In contrast, telogen effluvium often occurs suddenly following specific triggers, causing widespread shedding that can be alarming for those experiencing it.
Understanding the key differences between these conditions is crucial for obtaining proper diagnosis and pursuing effective treatment. Many women struggle to identify which type of hair loss they’re experiencing, leading to delays in appropriate care and unnecessary anxiety about their condition.
This comprehensive guide provides essential information to help you distinguish between female pattern hair loss and telogen effluvium. We’ll explore the unique characteristics of each condition, examine the visual signs and symptoms to watch for, and discuss diagnostic methods that healthcare professionals use to diagnose telogen effluvium and other hair loss conditions. Additionally, we’ll cover treatment options available for each condition, prevention strategies for maintaining optimal hair health, and guidance on when to consult with medical professionals for proper evaluation and care.
Key Takeaways – TL/DR
- Female pattern hair loss is a genetic condition causing gradual thinning, while telogen effluvium is temporary widespread shedding triggered by stress or illness
- Telogen effluvium typically occurs 2-3 months after a triggering event and affects the entire scalp, whereas female pattern baldness follows a specific pattern
- Acute telogen effluvium usually resolves within 6 months, while chronic telogen effluvium and female pattern hair loss require long-term management
- Professional diagnosis is essential as treatments differ significantly between conditions
Understanding Female Pattern Hair Loss
Female pattern hair loss represents the most common form of hair loss affecting women worldwide, characterized by progressive thinning that typically begins during reproductive years and accelerates after menopause. This condition, medically known as androgenetic alopecia, affects approximately 40% of women by age 50 and involves a complex interplay of genetic predisposition, hormonal sensitivity, and aging processes that gradually compromise hair follicle function.
What is Female Pattern Hair Loss
Female pattern hair loss, also called androgenetic alopecia or female pattern baldness, is a hereditary condition characterized by the gradual miniaturization of hair follicles in response to androgenic hormones. Unlike male pattern hair loss, which typically presents with distinct balding patterns, women experience more diffuse thinning across the crown and top of the scalp. The condition develops due to genetic predisposition combined with sensitivity to dihydrotestosterone (DHT), a potent androgen that causes hair follicles to shrink progressively over time. This process occurs gradually, often taking years or decades to become noticeable, making early detection and intervention crucial for optimal treatment outcomes.
Causes and Risk Factors
The primary cause of androgenic alopecia involves inherited sensitivity to DHT, which binds to androgen receptors in hair follicles and triggers a cascade of events leading to follicular miniaturization. Genetic factors play a dominant role, with studies showing that the condition can be inherited from either parent, with multiple genes contributing to susceptibility [1]. Family history remains the strongest predictor, as women with affected relatives have significantly higher risk of developing the condition. Hormonal changes throughout a woman’s life, including pregnancy, menopause, and thyroid disorders, can accelerate hair loss progression. Additional risk factors include certain medications, nutritional deficiencies, chronic stress, and underlying medical conditions that affect hormone levels or hair follicle health.
Progression Pattern
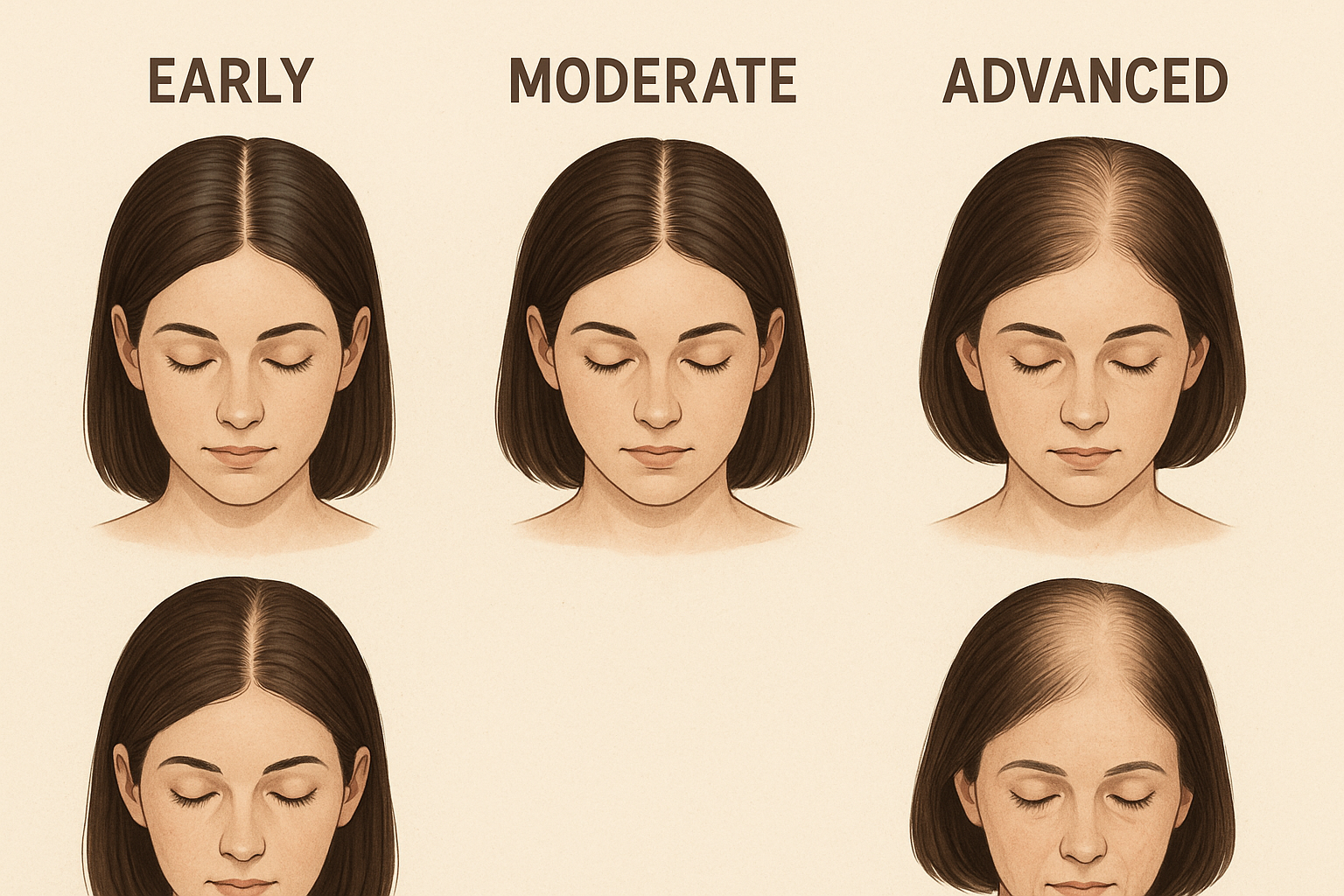
Female pattern baldness typically follows a predictable progression pattern that differs markedly from male pattern hair loss. The condition usually begins with gradual thinning at the crown and widening of the central part, while the frontal hairline generally remains intact. Most women notice increased hair shedding initially, followed by visible thinning in the central scalp region. The Ludwig classification system describes three stages of progression, from mild diffuse thinning to more pronounced crown baldness with maintained frontal and temporal hairlines. Unlike men, women rarely experience complete baldness, but the psychological impact can be equally significant due to the cultural importance of hair in feminine identity and appearance.
Understanding Telogen Effluvium
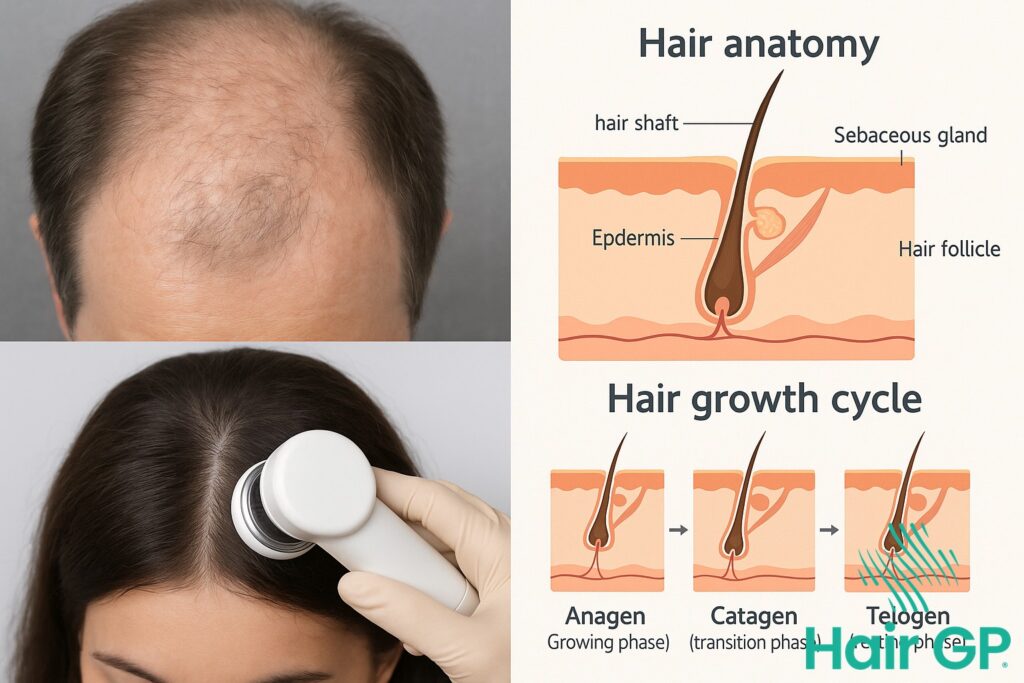
Telogen effluvium represents one of the most common forms of temporary hair loss affecting women, characterized by widespread hair shedding that disrupts the normal hair growth cycle. This condition occurs when hair follicles prematurely enter the resting telogen phase, leading to increased shedding that can be distressing but is typically reversible with proper understanding and management.
What is Telogen Effluvium
Telogen effluvium is a temporary condition that causes diffuse hair shedding across the scalp when the normal hair growth cycle becomes disrupted. Unlike pattern hair loss, this condition affects hair follicles uniformly, causing them to shift prematurely from the growing anagen phase into the resting telogen phase. During a normal hair growth cycle, approximately 10-15% of hair follicles remain in the telogen phase, which typically lasts 2-3 months [2]. However, in telogen effluvium, this percentage can increase dramatically to 30% or more, resulting in noticeable hair shedding that exceeds the normal rate of 50-100 hairs per day [3]. The condition manifests as widespread thinning rather than localized bald patches, affecting the entire scalp uniformly.
Types: Acute vs Chronic
Acute telogen effluvium typically develops suddenly following a specific trigger event, with hair shedding beginning 2-4 months after the initial stressor. This form usually resolves within 6 months once the underlying cause is addressed, allowing the hair growth cycle to return to normal patterns. The shedding in acute cases often appears dramatic but represents a temporary disruption that responds well to trigger identification and management.
Chronic telogen effluvium, defined as persistent diffuse hair shedding lasting longer than 6 months [4], presents a more complex clinical picture. This form may involve fluctuating periods of increased shedding interspersed with recovery phases, creating an ongoing cycle that can persist for years. Chronic cases often require more comprehensive evaluation to identify multiple contributing factors or underlying conditions that perpetuate the hair cycle disruption.
Common Triggers
Physical stress represents a primary trigger for telogen effluvium episodes, including major surgery, severe illness, high fever, or significant weight loss. Emotional trauma such as grief, divorce, or job loss can similarly disrupt the hair growth cycle through stress hormone elevation.
Medications frequently trigger telogen effluvium, particularly blood thinners, antidepressants, and hormonal contraceptives. Nutritional deficiencies, especially involving iron, protein, or essential vitamins, can also precipitate episodes by compromising follicle function and disrupting normal hair cycle progression.

Key Differences Between Female Pattern Hair Loss and Telogen Effluvium
Distinguishing between female pattern hair loss and telogen effluvium is essential for proper diagnosis and management, as these two conditions present with distinctly different characteristics despite both causing hair thinning in women. While both conditions can cause significant distress, understanding their unique features regarding onset, distribution patterns, and prognosis enables accurate identification and appropriate expectations for recovery.
Timeline and Onset
The timeline and onset represent the most striking differences between female pattern hair loss and telogen effluvium. Female pattern hair loss develops gradually over months to years, with hair thinning progressing slowly and often going unnoticed until significant miniaturization has occurred. This condition typically begins in a woman’s twenties or thirties, though it can manifest at any age after puberty, with onset often correlating with hormonal changes during menopause.
In contrast, telogen effluvium presents with sudden, dramatic hair loss that becomes apparent within two to four months following a triggering event. Common triggers include major surgery, severe illness, childbirth, extreme stress, rapid weight loss, or medication changes. This temporary hair loss condition can affect women of any age and often catches patients off-guard due to its rapid onset and the alarming amount of daily hair shedding.
Hair Loss Pattern
The distribution of hair loss provides another clear distinction between these conditions. Female pattern hair loss creates a characteristic pattern of thinning that primarily affects the crown and top of the scalp, with gradual widening of the central part. The frontal hairline typically remains intact, but the hair becomes progressively finer and shorter in affected areas due to follicular miniaturization.
Telogen effluvium, however, causes diffuse hair loss that affects the entire scalp uniformly. Women with this condition experience widespread hair thinning without the localized patterns seen in female pattern hair loss. The diffuse nature of telogen effluvium means that hair density decreases across all areas of the scalp, including regions that typically remain unaffected in pattern hair loss.
Reversibility
The prognosis and reversibility potential differ dramatically between these conditions. Female pattern hair loss represents a progressive, permanent condition where affected hair follicles undergo irreversible miniaturization. Without intervention, hair thinning continues over time, and complete restoration of original hair density rarely occurs naturally.
Conversely, telogen effluvium is typically a temporary hair loss condition with excellent recovery potential. Once the underlying trigger is identified and resolved, hair regrowth usually begins within three to six months, with complete recovery expected within six to twelve months. This fundamental difference in reversibility makes accurate diagnosis crucial for setting realistic expectations and determining appropriate management strategies for each condition.

Visual Signs and Symptoms to Spot
Recognizing the visual and physical signs of hair loss conditions enables early intervention and appropriate treatment. Each type of hair loss presents distinct patterns and characteristics that can be identified through careful observation of scalp appearance, hair texture changes, and specific shedding patterns.
Female Pattern Hair Loss Warning Signs
Female pattern hair loss typically begins with subtle changes that gradually become more pronounced. The most characteristic sign is crown thinning, where hair density decreases at the top and crown of the head while maintaining the frontal hairline. Women often notice their part widening progressively, making the scalp more visible through the hair. Unlike male pattern baldness, women rarely develop distinct bald spots but instead experience diffuse thinning across the crown area.
A key indicator involves miniaturized hair, where individual strands become progressively thinner, shorter, and lighter in color. These miniaturized hairs may appear almost transparent and lack the strength of normal hair. The scalp may appear more visible, particularly under bright lighting, and styling becomes increasingly difficult as hair volume decreases. Some women notice increased hair loss during washing or brushing, though this tends to be gradual rather than dramatic.
Telogen Effluvium Warning Signs
Telogen effluvium presents distinctly different visual signs characterized by widespread shedding affecting the entire scalp. The most alarming indicator is finding excessive hair on pillow cases, in shower drains, or on clothing throughout the day. This condition involves uniform thinning across all areas of the scalp, rather than the localized patterns seen in androgenetic alopecia.
Individuals experiencing telogen effluvium often report rapid hair loss that seems to occur suddenly, typically 2-4 months after a triggering event. The hair that sheds usually appears normal in thickness and length, distinguishing it from the miniaturized hair seen in pattern hair loss. The scalp itself typically appears healthy without inflammation or scarring. Hair shedding may be particularly noticeable during hair washing, with significantly more strands than usual coming out during shampooing and conditioning.
When Hair Loss is Normal vs Concerning
Understanding normal daily hair shedding helps distinguish between typical hair loss and concerning patterns. Healthy individuals lose approximately 50-100 hairs per day as part of the natural hair growth cycle[1]. Seasonal variations can increase this number slightly, with some people experiencing increased hair shedding during autumn months.
Concerning patterns include sudden increases in daily hair loss exceeding 150-200 strands, persistent thinning hair lasting several months, or development of any bald spots or receding hairline in women. Additional warning signs include changes in hair texture, decreased hair density making the scalp visible, or hair that breaks easily and appears weak. Any sudden onset of rapid hair loss, especially following illness, medication changes, or significant stress, warrants attention. Professional evaluation becomes essential when hair shedding continues beyond six months or when psychological distress accompanies the hair loss.

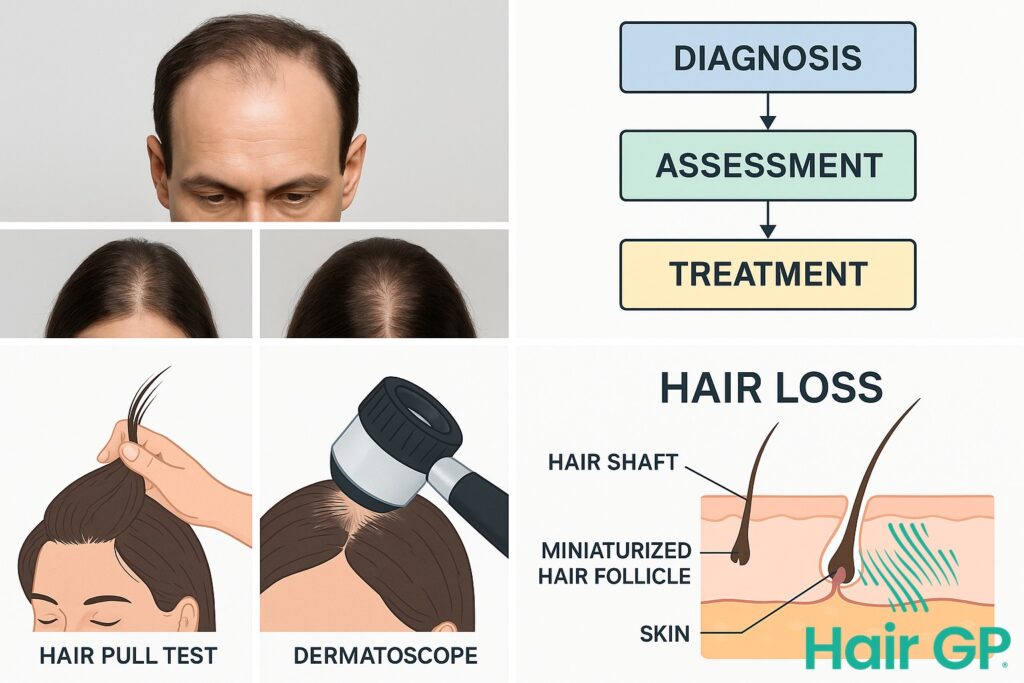
Diagnostic Methods and Tests
Professional diagnosis of hair loss conditions requires a systematic approach combining clinical examination, detailed medical history, and specialized testing procedures. Healthcare providers utilize multiple diagnostic methods to accurately identify the underlying cause of alopecia and distinguish between different types of hair loss conditions. This comprehensive evaluation ensures appropriate treatment recommendations and helps patients understand their specific condition.
Physical Examination
Specialist hair doctors begin the diagnostic process with a thorough physical examination of the scalp hair and hair follicles. The pull test represents a fundamental diagnostic technique where the physician gently grasps approximately 60 hairs between thumb and forefinger, applying steady traction to assess hair shedding patterns. In healthy hair conditions, fewer than 10% of hairs should be extracted during this procedure [5]. Visual inspection of the scalp reveals important clues about inflammation, scarring, or follicular damage that may indicate specific types of alopecia. Hair density assessment involves systematic evaluation of different scalp regions to identify patterns of thinning or areas where hair follicles have ceased producing healthy hair strands.
Medical History Assessment
Comprehensive medical history evaluation plays a crucial role in determining how to diagnose telogen effluvium and other hair loss conditions. Family history assessment helps identify genetic predisposition to pattern hair loss, while detailed medication review reveals potential pharmaceutical triggers for hair shedding. Physicians inquire about recent physical or emotional stress factors, surgical procedures, dietary changes, and hormonal fluctuations that commonly precipitate telogen effluvium. Timeline establishment proves essential, as telogen effluvium diagnosed through history typically shows hair loss beginning 2-4 months after a triggering event. Healthcare providers also evaluate menstrual history, pregnancy status, and thyroid symptoms to identify underlying medical conditions affecting hair follicles.
Laboratory Tests and Biopsies
Specialized diagnostic tests provide definitive confirmation when clinical examination suggests specific alopecia subtypes. Trichoscopy, also known as dermoscopy of hair and scalp, offers magnified visualization of hair follicles and scalp structures with diagnostic accuracy rates exceeding 85% for various alopecia conditions [6]. Blood tests commonly include full blood count, thyroid function studies, iron levels, and hormonal assessments to identify systemic causes of hair loss. Scalp biopsy remains the gold standard for diagnosing scarring alopecia and distinguishing between inflammatory and non-inflammatory hair loss conditions. This procedure involves removing a small tissue sample containing hair follicles for microscopic examination. When telogen effluvium diagnosed clinically remains uncertain, these specialized tests help confirm the diagnosis and guide appropriate treatment strategies for restoring healthy hair growth patterns.

Treatment Options for Each Condition
Effective management of hair loss requires understanding the distinct treatment approaches for each condition. While female pattern hair loss typically requires long-term medical intervention to slow progression and promote regrowth, telogen effluvium often resolves with identification and correction of underlying triggers combined with supportive care measures.
Female Pattern Hair Loss Treatments
Medical treatments to treat female pattern baldness focus on interrupting the hormone-driven miniaturization process. Topical minoxidil remains the first-line therapy, with 5% formulations demonstrating significant hair regrowth in 60-70% of women after 6-12 months of consistent use [7]. The medication works by extending the anagen phase and increasing blood flow to hair follicles, effectively promoting hair growth in thinning areas.
Oral finasteride, while primarily used in men, shows promise for postmenopausal women with androgenetic alopecia when used under careful medical supervision. Anti-androgen medications like spironolactone may also help by blocking dihydrotestosterone receptors at the follicle level.
Advanced hair loss treatments include hair transplantation procedures, which relocate healthy follicles from donor areas to thinning regions. Platelet-rich plasma (PRP) therapy has gained popularity as a minimally invasive option, with studies showing improved hair density and thickness in many patients [8]. Microneedling combined with topical treatments can enhance absorption and stimulate natural healing responses.
Telogen Effluvium Management
The approach to treat telogen effluvium centers on identifying and addressing underlying triggers while supporting optimal conditions for new hair growth. Since this condition often stems from stress, nutritional deficiencies, hormonal changes, or medication side effects, comprehensive evaluation of potential causes is essential.
Nutritional support plays a crucial role in telogen effluvium recovery. Ensuring adequate protein intake, iron levels, vitamin D, and B-complex vitamins provides the building blocks necessary for healthy hair regrowth. Supplements may be recommended when dietary intake proves insufficient or when deficiencies are identified through blood testing.
Gentle hair care practices become particularly important during the recovery phase. This includes using sulfate-free shampoos, minimizing heat styling, avoiding tight hairstyles, and being patient with the natural shedding process. Scalp massage and stress reduction techniques may help create optimal conditions for follicle recovery.
When to Expect Results
Hair regrowth timelines vary significantly between conditions and treatment approaches. For female pattern hair loss, patients should expect gradual improvement over 6-12 months with consistent treatment. Initial results may include reduced shedding before visible regrowth becomes apparent.
Telogen effluvium typically shows spontaneous improvement within 3-6 months once triggering factors are addressed. However, it may take 6-12 months for hair density to fully normalize as the hair growth cycle completes its phases. Monitoring progress through clinical photography and measurement tools helps track improvement and adjust treatment approaches when necessary. Realistic expectations and patience remain key components of successful hair loss treatments, as follicle recovery follows natural biological timelines that cannot be significantly accelerated.
Prevention and Hair Health Strategies
Maintaining healthy hair requires a comprehensive approach that addresses both internal and external factors affecting hair growth and retention. Evidence-based prevention strategies focus on optimizing nutrition, managing lifestyle factors, and implementing proper hair care practices to minimize the risk of excessive hair loss and promote optimal follicular function.
Lifestyle Factors
Daily habits significantly influence hair health, with chronic stress being a primary contributor to temporary hair loss conditions. Elevated cortisol levels from prolonged stress can cause hair follicles to enter the resting phase prematurely, leading to increased shedding and situations where hair stops growing normally. Implementing stress reduction techniques such as meditation, regular exercise, and adequate sleep helps maintain hormonal balance essential for healthy hair growth cycles.
Quality sleep plays a crucial role in cellular repair and regeneration processes that affect hair follicles. Adults should aim for 7-9 hours of consistent sleep to support optimal hair growth patterns and prevent unnecessary hair loss. Regular physical activity improves circulation to the scalp, delivering essential nutrients to hair follicles while reducing stress hormones that can negatively impact hair health.
Proper hair care practices prevent mechanical damage that leads to traction alopecia and breakage. Avoiding tight hairstyles, excessive heat styling, and harsh chemical treatments helps preserve hair integrity. Gentle brushing techniques and protective styling methods reduce the likelihood that individuals will lose hair due to physical trauma to the hair shaft and follicles.
Nutritional Support
Adequate protein intake forms the foundation of healthy hair, as hair follicles require amino acids for keratin production. Adults should consume approximately 0.8-1.2 grams of protein per kilogram of body weight daily to support optimal hair growth [2]. Insufficient protein intake can cause hair to shed hair excessively and enter telogen phase prematurely.
Essential vitamins and minerals play critical roles in preventing hair loss and maintaining follicular health. Iron deficiency represents one of the most common nutritional causes of hair loss, particularly in women, with studies showing that low ferritin levels correlate with increased hair shedding [1]. Vitamin D, B-complex vitamins, and zinc deficiencies can also disrupt normal hair growth cycles and contribute to various forms of alopecia.
A balanced diet rich in omega-3 fatty acids, biotin, and antioxidants supports scalp health and reduces inflammation that can impair follicular function. Incorporating foods such as fatty fish, nuts, seeds, leafy greens, and lean proteins provides the nutritional foundation necessary for maintaining strong, healthy hair throughout different life stages.

When to Consult a Healthcare Professional
While temporary hair shedding can often resolve naturally, certain circumstances warrant immediate professional evaluation to prevent further hair loss and address underlying health concerns. Recognizing the difference between normal hair fluctuations and serious medical conditions is crucial for timely intervention. Professional medical assessment becomes essential when hair loss patterns suggest autoimmune disorders, hormonal imbalances, or other systemic health issues requiring specialized treatment.
Red Flags That Require Immediate Attention
Several warning signs indicate that hair loss may stem from serious underlying conditions requiring urgent medical evaluation. Sudden severe hair loss occurring over days or weeks, rather than the gradual thinning typical of androgenetic alopecia, signals potential medical emergencies. This rapid onset differs significantly from normal shedding patterns and may indicate autoimmune conditions, severe nutritional deficiencies, or toxic exposures.
Patchy baldness presents another critical warning sign, particularly when accompanied by smooth, round areas of complete hair absence. These symptoms often indicate alopecia areata, an autoimmune condition where the immune system attacks hair follicles. Without proper medical intervention, alopecia areata can progress to alopecia totalis, resulting in complete scalp hair loss, or even alopecia universalis, affecting all body hair.
Scalp inflammation, including redness, scaling, pustules, or tender areas, requires immediate dermatological attention. These symptoms may indicate infections, inflammatory conditions, or scarring alopecia that can cause permanent hair follicle damage if left untreated. Additionally, hair loss accompanied by fever, fatigue, joint pain, or other systemic symptoms suggests underlying autoimmune or inflammatory conditions necessitating comprehensive medical evaluation.
Finding the Right Specialist
Selecting the appropriate healthcare provider significantly impacts diagnostic accuracy and treatment outcomes for hair loss conditions. Proper preparation enhances appointment effectiveness and diagnostic accuracy. Compile a comprehensive hair loss timeline, noting onset patterns, triggers, family history, medications, recent life changes, and accompanying symptoms. Bring photographs documenting hair loss progression, as visual documentation helps specialists assess severity and patterns over time.
Essential questions for specialists include asking about diagnostic tests needed, expected timeline for results, treatment options available, potential side effects, and prognosis for hair regrowth. Inquire about lifestyle modifications that might support recovery and whether temporary hair shedding patterns suggest reversible conditions or permanent changes requiring ongoing management strategies.

Conclusion
Understanding the distinction between female pattern hair loss and telogen effluvium represents a critical step in achieving optimal hair health outcomes. These two conditions, while both causing significant hair loss in women, require fundamentally different approaches to treatment and management.
Female pattern baldness demands long-term commitment and ongoing intervention to slow progression and maintain existing hair density. Without proper treatment, this chronic condition continues to worsen over time, making early recognition and intervention essential for preserving hair health.
In contrast, telogen effluvium often resolves naturally once underlying triggers are identified and addressed. This temporary condition typically improves within months, offering a more optimistic prognosis for complete recovery.
The ability to accurately diagnose telogen effluvium versus female pattern hair loss significantly impacts treatment success and patient expectations. Professional evaluation ensures appropriate therapeutic selection, whether addressing hormonal factors in pattern baldness or eliminating stressors causing telogen effluvium.
Women experiencing hair loss should seek prompt medical consultation rather than attempting self-diagnosis. Early intervention prevents unnecessary progression in chronic conditions while providing reassurance when temporary hair loss is involved. Understanding these fundamental differences empowers women to make informed decisions about their hair health and pursue timely, appropriate care for optimal outcomes.
Frequently Asked Questions
Acute telogen effluvium typically resolves within 6 months once the triggering factor is addressed. However, it may take up to 12-18 months to see full hair regrowth. Chronic telogen effluvium can persist longer and may require ongoing management.
Female pattern hair loss cannot be completely reversed, but its progression can be slowed or stopped with appropriate treatment. Some women may experience modest regrowth with treatments like minoxidil, but the condition is generally progressive without intervention.
Yes, it’s possible to have both female pattern hair loss and telogen effluvium simultaneously. This can make diagnosis more challenging and may require specialized testing to distinguish between the two contributing factors.
Common triggers include severe physical or emotional stress, major surgery, rapid weight loss, childbirth, medication changes, nutritional deficiencies, and hormonal changes. The hair loss typically occurs 2-3 months after the triggering event.
References
- Heilmann-Heimbach S, Herold C, Hochfeld LM, et al. Meta-analysis identifies novel risk loci and yields systematic insights into the biology of male-pattern baldness. Nat Commun. 2017;8(1):14694.
- Harries MJ, Paus R. The Pathogenesis of Primary Cicatricial Alopecias. Am J Pathol. 2010;177(5):2152-2162.
- Malkud S. Telogen Effluvium: A Review. J Clin Diagn Res. 2015;9(9):WE01-WE03.
- Rebora A. Telogen effluvium: a comprehensive review. Clin Cosmet Investig Dermatol. 2019;12:583-590.
- Spano F, Donovan JC. Alopecia areata: Part 1: pathogenesis, diagnosis, and prognosis. Can Fam Physician. 2015;61(9):751-755.
- Rudnicka L, Olszewska M, Rakowska A. Trichoscopy: how it may help the clinician. Dermatol Clin. 2013;31(1):29-41.
- Adil A, Godwin M. The effectiveness of treatments for androgenetic alopecia: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(1):136-141.e5.
- Fabbrocini G, Cantelli M, Masarà A, Annunziata MC, Marasca C, Cacciapuoti S. Female pattern hair loss: A clinical, pathophysiological and therapeutic review. Int J Womens Dermatol. 2018;4(4):203-211.