Introduction
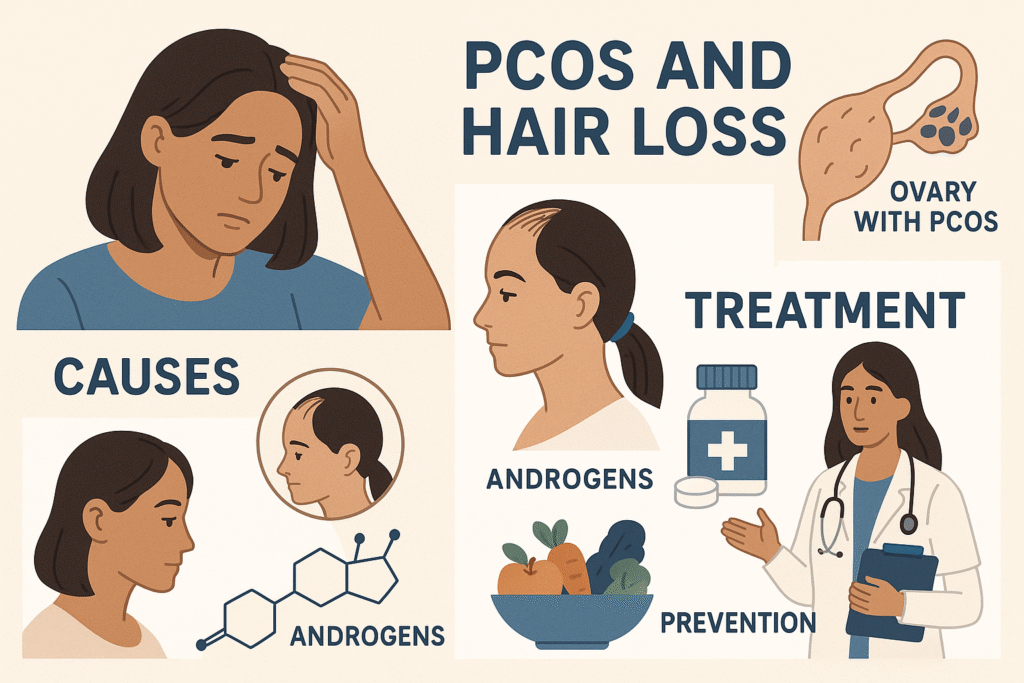
Polycystic ovary syndrome (PCOS) affects millions of women worldwide, making it one of the most common hormonal disorders of reproductive age. While many are familiar with PCOS symptoms like irregular periods and weight gain, fewer understand the profound impact this condition can have on hair health. For many women living with PCOS, hair loss represents one of the most emotionally challenging and visible aspects of their diagnosis.
The connection between PCOS and hair loss stems from the hormonal imbalance that fundamentally defines this condition. Women with PCOS often produce excess androgens, male hormones that can dramatically disrupt normal hair growth cycles. This hormonal disruption frequently leads to androgenic alopecia, commonly known as female pattern baldness, where hair gradually thins and falls out in predictable patterns across the scalp.
PCOS hair loss isn’t just about losing hair – it’s about understanding how your body’s complex hormonal systems interact and affect your overall well-being. The encouraging news is that with proper knowledge and appropriate treatment, many women find effective ways to manage and even reverse hair loss associated with their condition.
This comprehensive guide will help you understand the fundamental relationship between PCOS and hair loss, recognize the different types and patterns of hair loss that can occur, identify key symptoms and warning signs, navigate the diagnostic process with healthcare providers, explore various medical and lifestyle treatment options, and discover evidence-based lifestyle changes that can make a meaningful difference in your hair health journey.
Key Takeaways – TL/DR
- PCOS directly causes hair loss through elevated androgen levels that shrink hair follicles
- Female pattern baldness from PCOS typically affects the crown and frontal areas of the scalp
- Early diagnosis and treatment can slow progression and potentially restore some hair growth
- Multiple treatment options exist including medications, lifestyle changes, and topical treatments
Understanding the PCOS-Hair Loss Connection
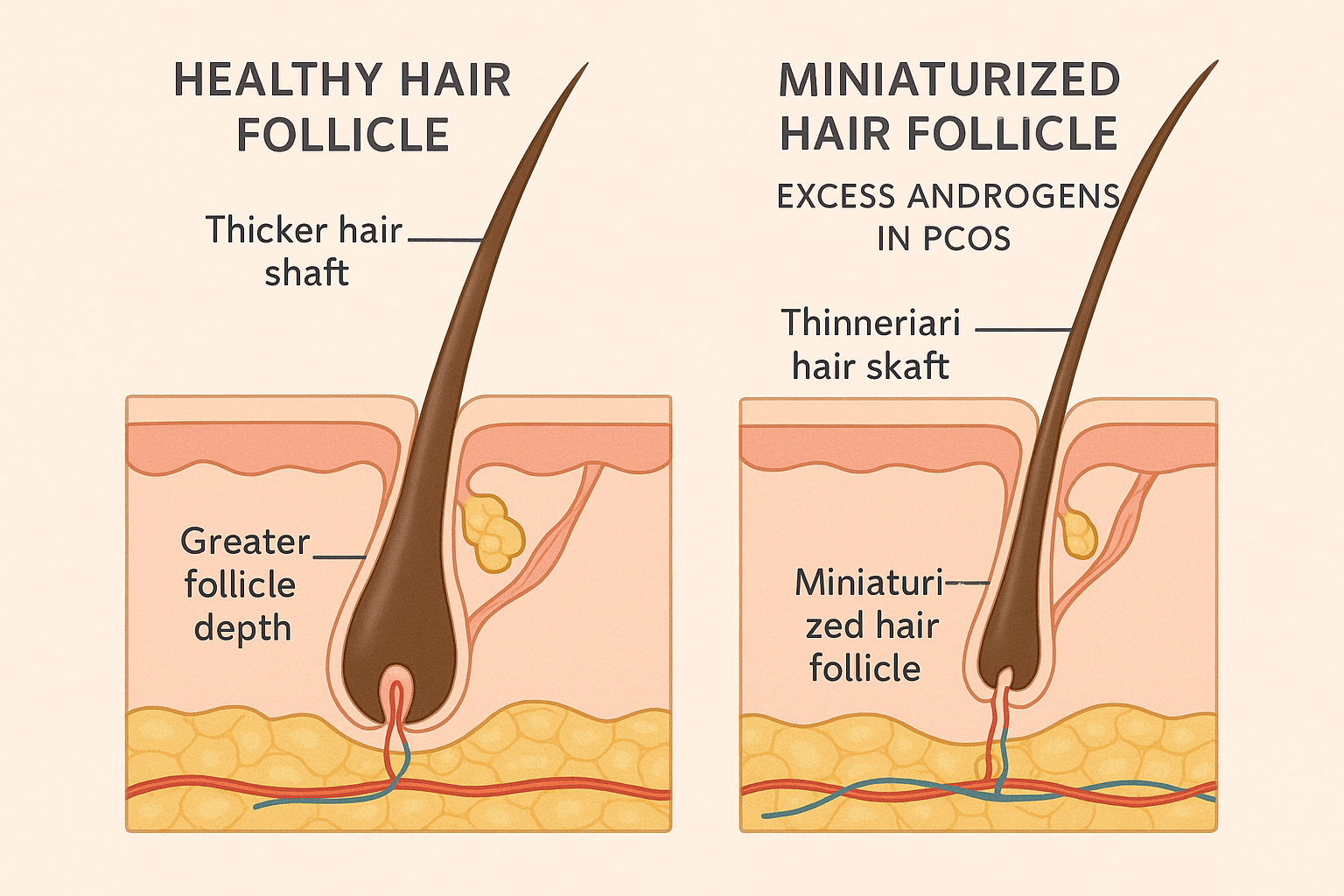
The relationship between polycystic ovaries and hair loss represents a complex interplay of hormonal imbalances that fundamentally disrupts normal hair growth cycles. Women with PCOS experience significantly elevated androgen levels, particularly testosterone and dihydrotestosterone (DHT), which directly impact hair follicles at the cellular level [1]. These excess androgens bind to androgen receptors in hair follicles, causing them to shrink progressively over time—a process known as follicular miniaturization.
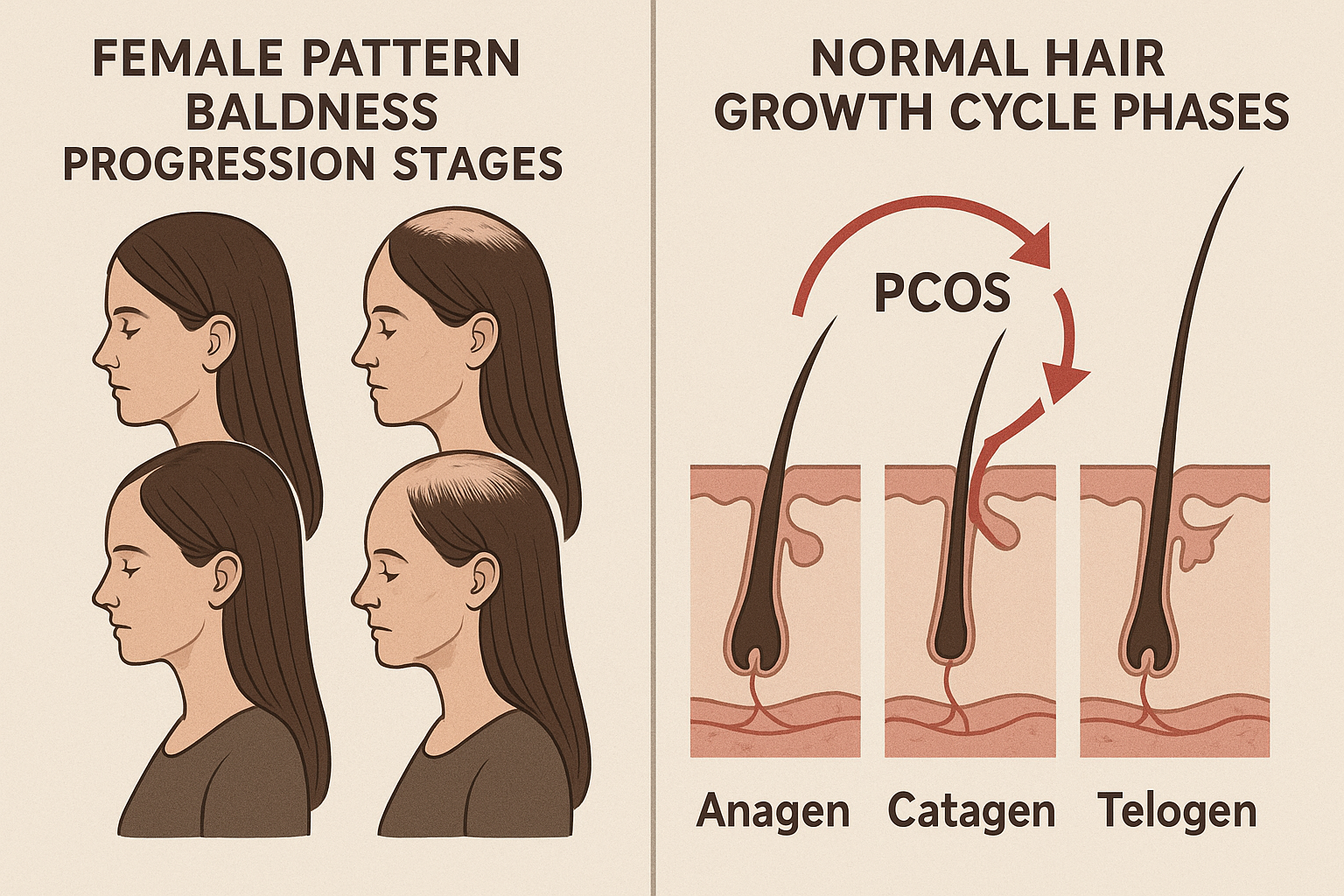
PCOS related hair loss typically manifests as androgenic alopecia, characterized by diffuse thinning across the crown and frontal scalp regions. This pattern differs from typical female pattern hair loss, often beginning earlier and progressing more rapidly. Research indicates that approximately 20-30% of women with PCOS experience clinically significant hair thinning [2]. The elevated androgen environment shortens the anagen (growth) phase of hair cycles while prolonging the telogen (resting) phase, resulting in weaker, shorter hair strands that eventually cease growing altogether.
Understanding this mechanism is crucial because it explains why conventional hair loss treatments may prove insufficient for women with PCOS. The underlying hormonal dysfunction requires targeted approaches that address both the excess androgens and their downstream effects on hair follicles, making PCOS-associated hair loss a unique clinical challenge.
How PCOS Triggers Different Types of Hair Loss
PCOS triggers hair loss through complex hormonal pathways that directly assault hair follicles and disrupt normal hair growth cycles. The elevated androgen levels characteristic of PCOS, combined with insulin resistance, create a perfect storm for follicle miniaturization and compromised hair growth patterns.
Androgenetic Alopecia in PCOS
Androgenetic alopecia represents the most prevalent form of hair loss in women with PCOS, affecting up to 70% of patients [3]. Unlike male pattern baldness, female pattern baldness in PCOS typically manifests as diffuse thinning across the crown and vertex regions while preserving the frontal hairline. The excess androgen hormones, particularly dihydrotestosterone (DHT), bind to sensitive hair follicles and systematically shrink them over time. This miniaturization process shortens the anagen growth phase while extending the telogen resting phase, resulting in progressively thinner, shorter hair strands. Insulin resistance compounds this damage by creating inflammatory conditions that further compromise follicle health and hair growth potential [4].
Telogen Effluvium and Stress-Related Loss
Many women with PCOS also experience telogen effluvium, characterized by diffuse hair shedding across the entire scalp. This pattern typically results from the chronic stress of hormonal fluctuations and metabolic dysfunction inherent in PCOS. Unlike androgenetic alopecia, telogen effluvium often presents as temporary hair loss, though repeated episodes can lead to permanent thinning if underlying hormonal imbalances remain unaddressed.
Recognizing PCOS Hair Loss Symptoms
Understanding the specific signs and patterns of PCOS-related hair loss helps distinguish it from other causes of hair thinning. PCOS symptoms affecting scalp hair follow distinctive patterns that develop gradually over time. Recognizing these early indicators allows for prompt intervention and better management outcomes.
Early Warning Signs
The first signs of PCOS-related hair thinning often begin subtly but become increasingly noticeable. Increased hair shedding becomes apparent during washing or brushing, with more strands collecting in drains, on pillows, and throughout your living spaces. A widening part line develops as the hairline begins to thin, particularly noticeable when styling hair in familiar ways. Reduced hair volume creates a less full appearance overall, even when using the same styling products and techniques that previously provided satisfactory results.
Advanced Thinning Patterns
As PCOS progresses without proper treatment, more pronounced thinning hair patterns emerge across the scalp. Crown thinning becomes increasingly visible, creating circular areas of reduced hair density at the top of the head. Vertex baldness may develop, following male-pattern baldness characteristics despite occurring in women. Miniaturized hair follicles produce progressively thinner, shorter strands that eventually stop producing visible hair altogether, leaving affected areas with sparse coverage.

Getting Diagnosed: PCOS and Hair Loss Evaluation
When experiencing hair loss alongside other symptoms like irregular menstrual cycles or weight gain, consulting a healthcare provider becomes essential to diagnose PCOS accurately. Healthcare professionals utilize comprehensive evaluation methods to determine whether PCOS related hair loss is the underlying cause of your symptoms. The diagnostic process typically begins with a detailed medical history and physical examination, focusing on signs of androgen excess and metabolic dysfunction.
Healthcare providers rely on the Rotterdam criteria to diagnose PCOS, which requires meeting two of three key conditions: irregular menstrual cycles or absence of ovulation, clinical or biochemical signs of elevated androgens, and polycystic ovaries visible on ultrasound [5]. This standardized approach ensures accurate diagnosis while ruling out other conditions that may mimic PCOS symptoms.
Hormonal testing forms the cornerstone of PCOS diagnosis, measuring testosterone, DHEA-S, and LH-to-FSH ratios to identify elevated androgen levels [6]. Additional blood work may include insulin levels, glucose tolerance tests, and thyroid function assessments. Pelvic ultrasounds examine the ovaries for characteristic cyst formations, while dermatological evaluations document hair loss patterns and other androgen-related symptoms to confirm the PCOS related connection.
Treatment Options for PCOS Hair Loss
Comprehensive treatment strategies for PCOS-related hair loss encompass medical interventions, topical applications, and advanced procedures that target the underlying hormonal imbalances and follicular damage. These evidence-based approaches work through different mechanisms to treat hair loss and restore follicular function, with success rates varying based on individual hormonal profiles and treatment adherence.
Topical Treatments and Medications
Minoxidil, marketed as Regaine, remains the gold standard topical treatment to stimulate hair growth in PCOS patients. Clinical studies demonstrate that 5% minoxidil solution produces significant hair regrowth in 65-70% of women with androgenetic alopecia when applied once daily [7]. The medication works by prolonging the anagen phase and increasing blood flow to follicles, with visible improvements typically emerging after 3-4 months of consistent use.
Hormonal Therapy Options
Oral contraceptives containing anti-androgenic progestins effectively reduce circulating androgen levels, while spironolactone blocks androgen receptors at the follicular level. Studies show that spironolactone therapy achieves hair regrowth or stabilization in approximately 80% of women with PCOS-related hair loss [8]. Finasteride may be considered for severe cases, though reproductive considerations limit its use in women of childbearing age.
Advanced Treatment Procedures
Platelet-rich plasma therapy shows promise for enhancing follicular regeneration, while hair transplantation offers permanent solutions for extensive hair loss but at Hair GP it would be the very last option after all others have been tried. Low-level laser therapy provides additional stimulation for compromised follicles in conjunction with medical treatments.

Lifestyle Changes and Prevention Strategies
Strategic lifestyle modifications can significantly support hair health while addressing underlying PCOS-related health conditions. These evidence-based interventions work synergistically with medical approaches to slow hair loss progression and improve overall well-being.
Dietary Modifications for Hair Health
Anti-inflammatory dietary patterns help manage PCOS symptoms and support hair health by reducing systemic inflammation [9]. Focusing on whole foods, lean proteins, and complex carbohydrates helps stabilize blood sugar levels, which directly impacts hormone balance and hair follicle health. Key nutrients including iron, zinc, biotin, and omega-3 fatty acids play crucial roles in maintaining healthy hair growth cycles. Avoiding processed foods and refined sugars helps prevent insulin spikes that can worsen androgenic effects on hair follicles, potentially reducing unwanted body hair growth while supporting scalp hair retention.
Stress Management and Sleep Hygiene
Chronic stress elevates cortisol levels, which can accelerate hair loss and worsen PCOS symptoms [10]. Regular stress reduction techniques such as meditation, yoga, or deep breathing exercises help lower cortisol and support mental health. Quality sleep of 7-9 hours nightly allows proper hormone regulation and hair follicle repair. Establishing consistent sleep schedules and creating relaxing bedtime routines can promote more hair growth and reduce stress-related hair loss progression.

Conclusion
PCOS hair loss represents a challenging but manageable condition affecting millions of women worldwide. Successfully addressing pcos related hair loss requires understanding that this condition responds well to comprehensive treatment approaches when properly managed by qualified healthcare professionals.
Early intervention plays a crucial role in preventing further hair loss and potentially reversing existing damage. Women experiencing pcos symptoms, particularly those noticing changes in hair density, should promptly consult with a healthcare provider specializing in hormonal disorders. These professionals develop personalized treatment plans addressing both underlying hormonal imbalances and visible hair loss manifestations.
Lifestyle modifications, including dietary changes, regular exercise, stress management, and targeted supplementation, work synergistically with medical treatments to optimize outcomes. The combination of hormonal therapies, topical treatments, and healthy lifestyle practices has shown remarkable success in restoring hair health for many women with PCOS.
Remember that pcos hair loss is not permanent—with proper medical guidance, patience, and commitment to treatment protocols, women can regain confidence while effectively managing their overall health.
Frequently Asked Questions
While PCOS hair loss can often be slowed and partially improved with proper treatment, complete reversal depends on factors like how long the condition went untreated and individual response to therapy. Early intervention typically yields better results.
Most treatments require 3-6 months to show initial results, with significant improvement typically visible after 6-12 months of consistent treatment. Hair regrowth is a gradual process that requires patience and adherence to treatment plans.
Weight loss can help improve PCOS symptoms including hair loss by reducing insulin resistance and lowering androgen levels. Even a 5-10% reduction in body weight can lead to meaningful improvements in hormonal balance.
References
- Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018;14(5):270-284.
- Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society Disease State Clinical Review: Guide to the Best Practices in the Evaluation and Treatment of Polycystic Ovary Syndrome – Part 2. Endocr Pract. 2015;21(12):1415-26.
- Carmina E, Azziz R, Bergfeld W, et al. Female pattern hair loss and androgen excess: a report from the multidisciplinary androgen excess and PCOS committee. J Clin Endocrinol Metab. 2019;104(7):2875-2891.
- Hoeger KM, Dokras A, Piltonen T. Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab. 2021;106(3):e1071-e1083.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19-25.
- Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602-1618.
- Adil A, Godwin M. The effectiveness of treatments for androgenetic alopecia: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(1):136-141.e5.
- Rathnayake D, Sinclair R. Use of spironolactone in dermatology. Skin Pharmacol Physiol. 2010;23(4):171-176.
- Barrea L, Marzullo P, Muscogiuri G, et al. Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr Res Rev. 2018;31(2):291-301.
- Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome. Hum Reprod. 2017;32(5):1075-1091.