Introduction
The pandemic brought unexpected health challenges beyond respiratory symptoms, with many COVID-19 survivors experiencing a surprising and distressing side effect: significant hair loss. This post-viral hair loss has emerged as one of the most commonly reported long-term effects of COVID-19 infection, affecting millions of people worldwide and causing considerable concern and anxiety.
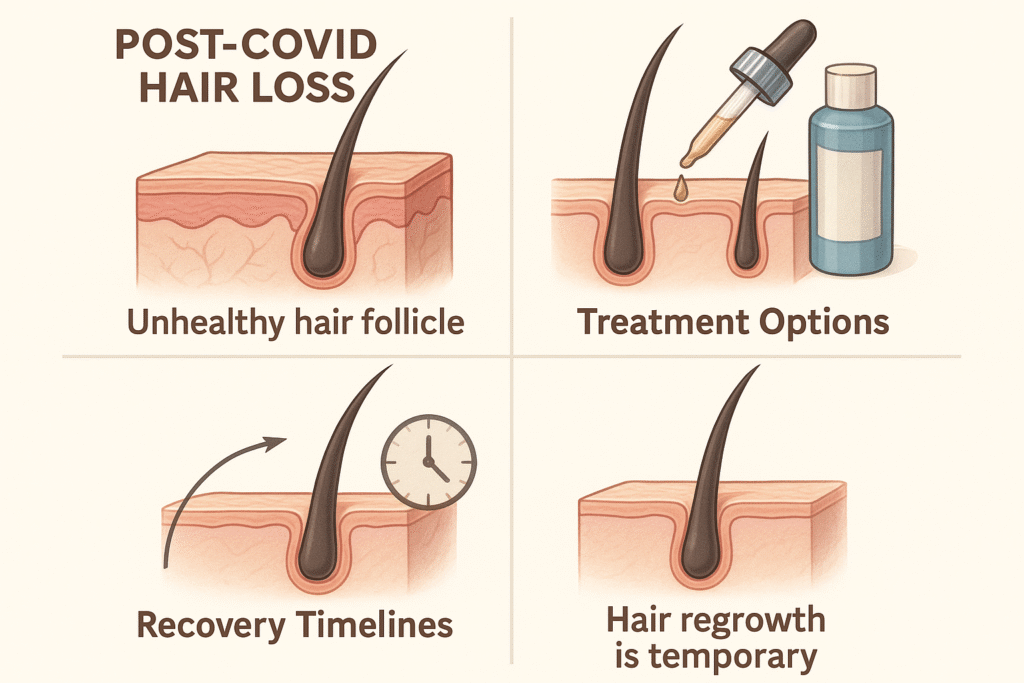
COVID hair loss typically manifests as increased shedding, thinning, or even patchy bald spots, with telogen effluvium being the most frequently observed pattern. This condition occurs when physical or emotional stress pushes hair follicles into a resting phase, leading to noticeable hair loss weeks or months after the initial trigger. While alarming for those experiencing it, understanding that this represents a normal biological response to severe illness can provide much-needed reassurance.
Various hair disorders can develop following COVID-19 infection, ranging from diffuse thinning to more localized patterns of hair loss. The good news is that most cases of post-viral hair loss are temporary and treatable, with proper understanding and intervention often leading to successful recovery.
This comprehensive guide explores the science behind why COVID-19 triggers hair loss, helping you identify different types and patterns of hair loss that may occur. We’ll examine the typical timeline from infection to hair loss onset, discuss the underlying biological mechanisms at work, and provide evidence-based treatment options and recovery strategies. Most importantly, we’ll outline realistic expectations for regrowth and prevention strategies to protect your hair health moving forward.
Key Takeaways – TL/DR
- COVID-19 can trigger temporary hair loss 2-4 months after infection, primarily through telogen effluvium
- Hair loss severity often correlates with disease severity and emotional stress levels during illness
- Most COVID-related hair loss is temporary and resolves within 6-12 months with proper care
- Multiple treatment options exist including topical minoxidil, lifestyle changes, and stress management
Understanding COVID-19 Related Hair Loss
Post-viral hair loss has emerged as a significant concern following COVID-19 infection, affecting a substantial portion of survivors months after their initial recovery. This phenomenon represents a form of stress-induced hair shedding that occurs when viral infections disrupt the body’s normal physiological processes, including the delicate balance of hair follicles and their growth patterns.
Prevalence and Demographics
Research indicates that approximately 25-30% of COVID-19 patients experience hair loss within 2-4 months of infection, making it one of the most common long-term symptoms of the pandemic [1]. Women are disproportionately affected, representing nearly 75% of reported cases of covid hair loss, though men and children also experience this condition. Interestingly, the severity of hair loss does not directly correlate with the initial severity of COVID-19 symptoms, meaning even individuals with mild or asymptomatic infections can develop significant hair shedding [2]. Age appears to be a factor, with adults between 30-60 years showing higher rates of post-viral hair loss compared to younger populations. Healthcare workers and individuals experiencing prolonged stress during the pandemic also report elevated rates of hair loss, suggesting multiple contributing factors beyond the viral infection itself.
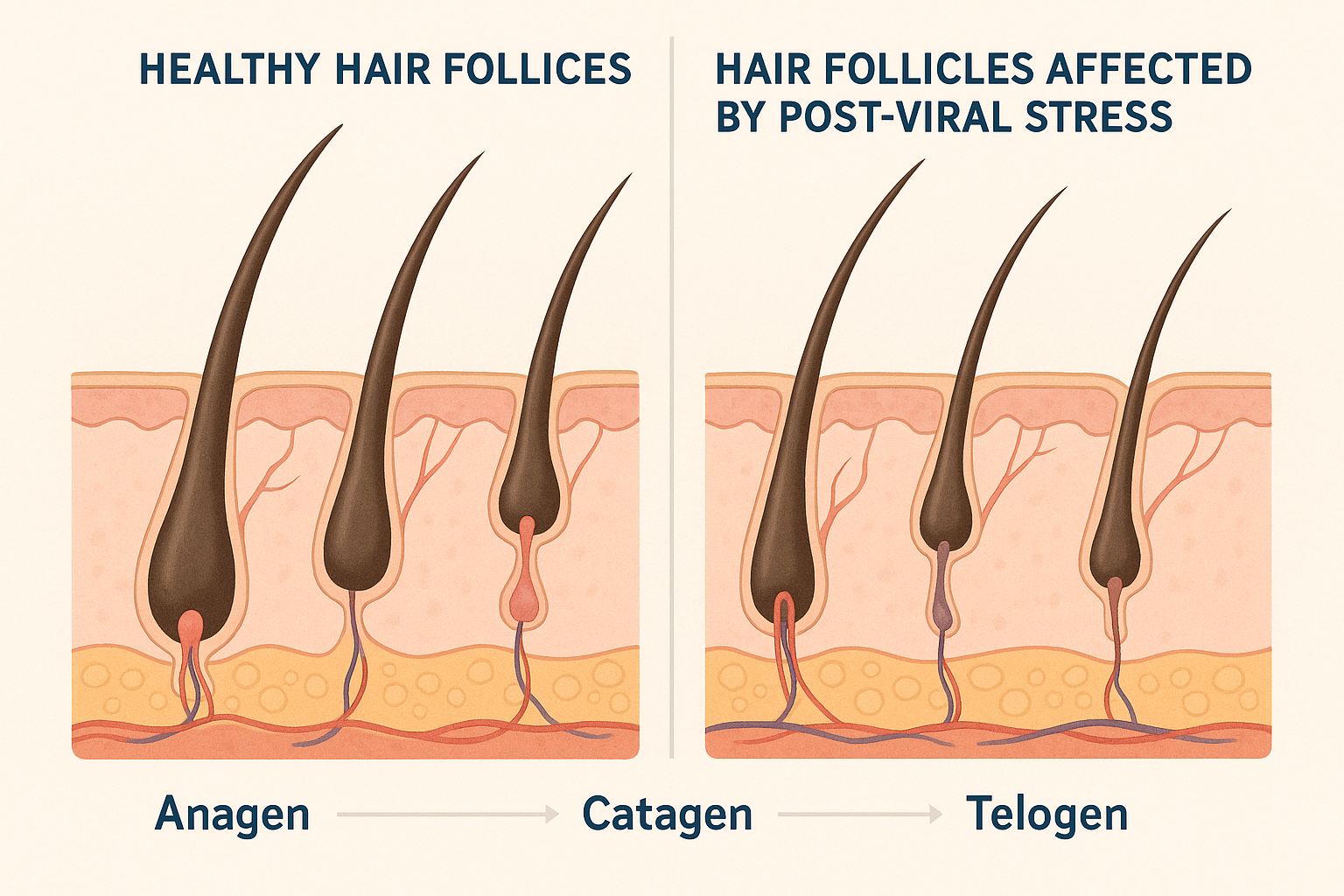
The Hair Growth Cycle Connection
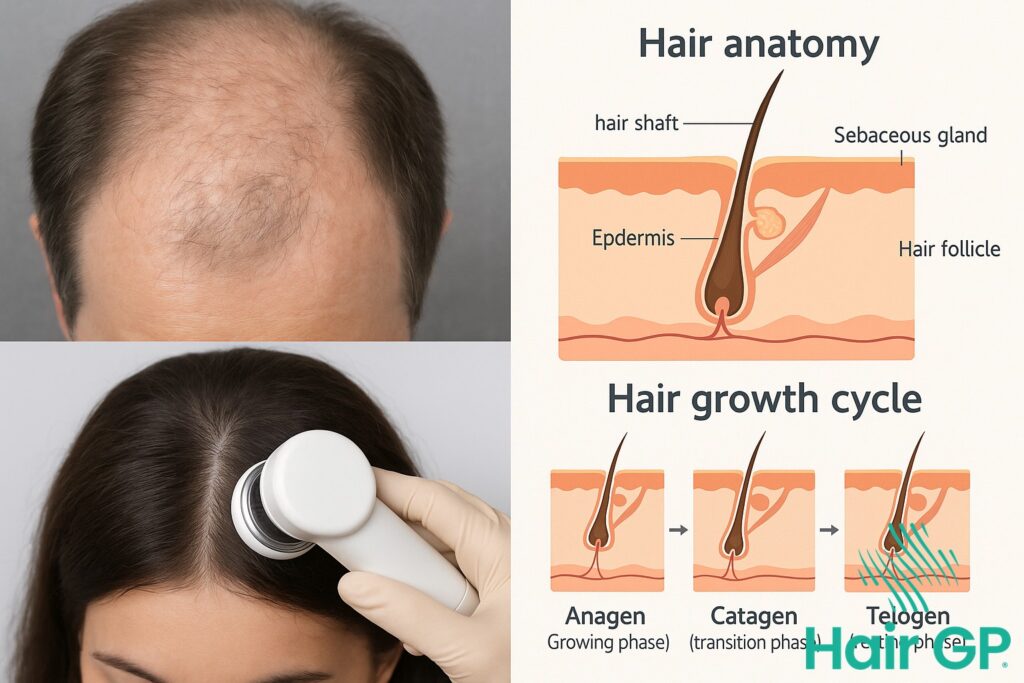
To understand covid hair loss, it’s essential to recognize how viral infections disrupt the normal hair growth cycle. Hair follicles naturally cycle through three phases: anagen (growth phase lasting 2-7 years), catagen (transitional phase lasting 2-3 weeks), and telogen (resting phase lasting 2-4 months). During normal conditions, approximately 85-90% of hair remains in the anagen phase while only 10-15% enters telogen. However, when the body experiences significant stress from viral infection, inflammatory responses, or fever, a phenomenon called telogen effluvium occurs [3]. This stress response pushes a larger percentage of hair follicles prematurely into the telogen phase, where hair stops growing and eventually sheds. The hair growth cycle disruption explains why post-viral hair loss typically appears 2-4 months after COVID-19 infection, as this represents the natural timeline for telogen hairs to be released from hair follicles. Understanding this biological mechanism helps explain why pandemic-related hair loss is usually temporary, as hair follicles can return to normal cycling patterns once the stress response subsides.
Types of Hair Loss After COVID-19
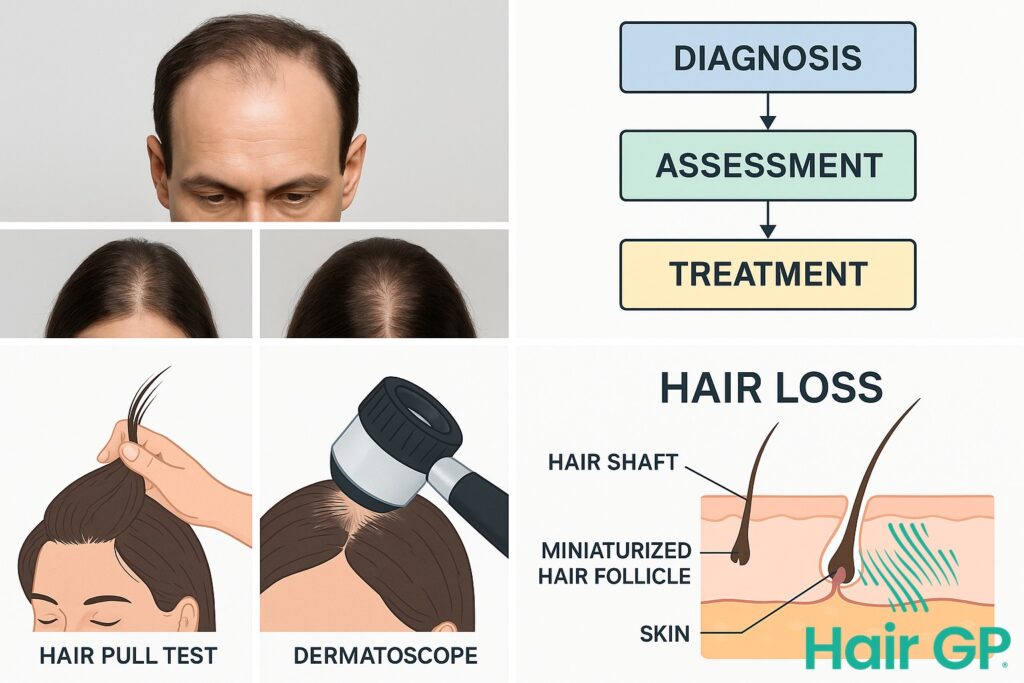
COVID-19 infection can trigger several distinct types of hair loss, each with unique characteristics and underlying mechanisms. Understanding these different patterns is crucial for recognizing the specific type affecting you and seeking appropriate treatment. Research has identified three primary categories of post-COVID hair loss, ranging from temporary diffuse shedding to more complex autoimmune-related patterns.
Telogen Effluvium: The Most Common Type
Telogen effluvium represents the most frequently observed form of COVID-related hair loss, affecting up to 25% of recovered patients [4]. This condition occurs when stress from viral infection pushes hair follicles prematurely into the resting phase, resulting in diffuse hair loss across the entire scalp. Acute telogen effluvium typically begins 2-4 months after COVID infection, characterized by excessive hair shedding of 100-400 strands daily compared to the normal 50-100 strands. The chronic form may persist for six months or longer, particularly in individuals experiencing prolonged COVID symptoms. Unlike patterned baldness, telogen effluvium causes uniform hair thinning without specific areas of concentration, making it relatively easy to distinguish from other types.
Alopecia Areata and Patchy Loss
Alopecia areata presents as distinct circular or oval patches of complete hair loss, often appearing suddenly within weeks of COVID infection [5]. This autoimmune condition occurs when the immune system, already activated by viral infection, mistakenly attacks hair follicles. The patches typically measure 1-4 centimeters in diameter and may appear anywhere on the scalp, though they commonly manifest near the hairline or crown. Unlike diffuse hair loss, alopecia areata creates sharply defined boundaries between affected and unaffected areas. In severe cases, the condition may progress to alopecia totalis, affecting the entire scalp, or alopecia universalis, involving all body hair. The autoimmune connection explains why individuals with existing autoimmune conditions show higher susceptibility to developing this pattern after COVID infection.
Androgenetic Alopecia Acceleration
COVID-19 can accelerate existing androgenetic alopecia, the genetic predisposition to male and female pattern baldness. Stress-induced hormonal changes, particularly elevated cortisol levels, can trigger dormant hair loss genes and accelerate the miniaturization process of hair follicles. This acceleration manifests differently in men and women: men typically experience receding hairlines and crown thinning, while women develop diffuse thinning across the top of the scalp. The distinguishing feature of accelerated androgenetic alopecia is its adherence to established genetic patterns rather than the random distribution seen in telogen effluvium. Hair thinning follows familiar family patterns, making it identifiable through comparison with relatives’ hair loss experiences.

Timeline and Symptoms of Post-COVID Hair Loss
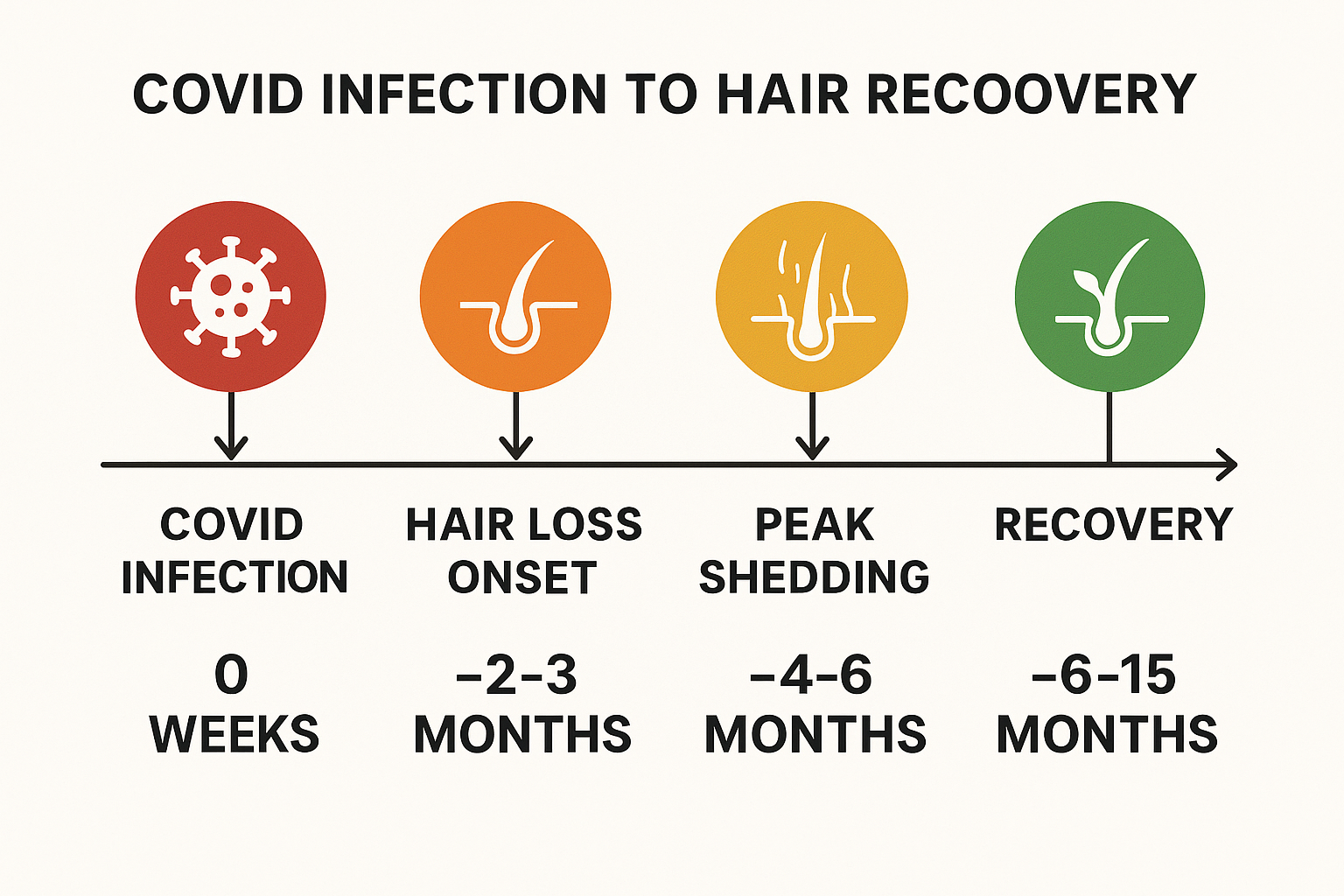
Understanding the timeline of post-COVID hair loss helps patients recognize symptoms and manage expectations during recovery. Most individuals who develop hair loss after COVID-19 infection will notice hair loss beginning approximately 2-4 months following their initial illness [6]. This delayed onset is characteristic of telogen effluvium, the most common type of hair loss associated with COVID-19, where the stress of illness pushes hair follicles into a resting phase before shedding occurs.
The progression typically follows a predictable pattern. Patients may initially observe increased hair fall during washing or brushing, which gradually intensifies over several weeks. Peak hair shedding usually occurs between 3-6 months post-infection, when individuals experience the most dramatic hair loss [7]. During this phase, many report losing 100-300 hairs daily compared to the normal 50-100 hairs, creating noticeable thinning particularly around the hairline, crown, and temples.
Beyond visible hair loss, many patients experience accompanying symptoms that can be equally distressing. An itchy scalp is commonly reported, often preceding or coinciding with excessive hair loss episodes. Some individuals describe scalp tenderness or sensitivity, making hair washing and styling uncomfortable. These sensations may fluctuate throughout the shedding period, with some patients noting that sudden shedding episodes correlate with increased scalp irritation.
The duration of active shedding varies considerably among individuals, typically lasting 3-6 months from onset. Most patients notice gradual improvement after the peak shedding period, with new hair growth becoming visible around 6-9 months post-infection. However, complete hair density recovery can take 12-18 months or longer. During the recovery phase, new hair may initially appear finer or different in texture before returning to normal characteristics. Recognizing these timeline patterns helps patients understand that while hair shedding can be alarming, it typically represents a temporary response to illness stress rather than permanent hair loss, providing reassurance during what can be an emotionally challenging experience.
Causes and Mechanisms Behind COVID Hair Loss
COVID-19 disrupts normal hair growth through complex biological mechanisms involving stress responses, immune activation, and inflammatory cascades. The virus doesn’t directly attack hair follicles, but rather creates systemic conditions that force follicles into premature dormancy. Understanding these interconnected pathways helps explain why hair loss caused by COVID-19 can persist long after recovery and varies significantly based on disease severity and individual immune responses.
Stress Response and Hormonal Changes
The physical trauma of COVID-19 infection activates the hypothalamic-pituitary-adrenal axis, leading to sustained cortisol elevation that can trigger hair loss by disrupting the normal hair growth cycle [8]. This stress hormone forces hair follicles to transition prematurely from the active growth phase into the telogen phase, where hair becomes dormant and eventually sheds. Beyond physical stress, the emotional stress associated with illness, hospitalization, and recovery concerns creates additional hormonal disruption. Prolonged elevation of stress hormones interferes with growth factors essential for maintaining healthy hair follicles, including insulin-like growth factor-1 and thyroid hormones. The severity and duration of stress responses often correlate with disease severity, explaining why patients who experienced more severe COVID-19 symptoms frequently report more extensive hair loss. Additionally, disrupted sleep patterns and nutritional deficiencies during illness compound these hormonal imbalances, further compromising hair follicle health and regenerative capacity.
Inflammatory and Immune Factors
COVID-19 triggers an intense inflammatory response characterized by elevated pro-inflammatory cytokines including interleukin-6, tumor necrosis factor-alpha, and interleukin-1β, which directly interfere with hair follicle cycling [9]. These inflammatory mediators create a hostile microenvironment around hair follicles, disrupting normal cellular communication and growth signals. The cytokine storm associated with severe COVID-19 cases can overwhelm the body’s anti-inflammatory mechanisms, leading to prolonged inflammatory conditions that extend hair loss duration. Immune system overstimulation also diverts essential nutrients and energy away from non-essential functions like hair growth toward fighting infection. The inflammatory cascade affects dermal papilla cells, which are crucial for hair follicle maintenance and regeneration. Additionally, oxidative stress from excessive inflammation damages hair follicle stem cells, potentially affecting future hair growth cycles. This inflammatory response explains why individuals with more robust immune reactions or pre-existing inflammatory conditions may experience more severe or persistent hair loss following COVID-19 infection.
Treatment Options and Recovery Solutions
Effective management of post-COVID hair loss requires a comprehensive approach combining medical interventions, lifestyle modifications, and appropriate professional guidance. Multiple treatment strategies can help stop hair loss and promote hair regrowth, with success rates varying based on individual factors and timing of intervention.
Medical Treatments and Therapies
Topical minoxidil remains the gold standard first-line treatment for promoting hair regrowth in post-COVID patients. Clinical studies demonstrate that minoxidil can effectively stimulate hair follicles and accelerate the recovery process [10]. The medication works by increasing blood flow to hair follicles and extending the growth phase of the hair cycle. Patients typically begin seeing initial results within 3-4 months of consistent use, with optimal regrowth occurring after 6-12 months of treatment.
For more severe cases, dermatologists may prescribe oral medications or recommend advanced therapies. Platelet-rich plasma (PRP) injections have shown promising results in accelerating hair regrowth by delivering concentrated growth factors directly to affected follicles [11]. Low-level laser therapy represents another emerging option that can complement topical treatments by stimulating cellular activity in hair follicles.
Lifestyle and Nutritional Support
Nutritional deficiencies often exacerbate post-COVID hair loss, making dietary intervention crucial for recovery. Essential nutrients for hair regrowth include iron, zinc, biotin, and vitamins D and B12. A balanced diet rich in lean proteins, leafy greens, and omega-3 fatty acids provides the building blocks necessary for healthy hair production.
Stress management plays a vital role in stopping ongoing hair loss and supporting recovery. Chronic stress can perpetuate telogen effluvium, making relaxation techniques, adequate sleep, and regular exercise important components of treatment. Gentle scalp massage can improve circulation and create an optimal environment for regrowth.
Proper scalp care involves using mild shampoos and avoiding excessive heat styling or chemical treatments during the recovery phase. Patients should handle their hair gently, avoiding tight hairstyles that create additional tension on vulnerable follicles.
When to Seek Professional Help
Consultation with a Hair Specialist Doctor becomes essential when hair loss persists beyond six months post-infection or when shedding exceeds normal recovery patterns [12]. Warning signs that warrant immediate professional evaluation include patchy hair loss, scalp inflammation, or complete absence of new growth after several months of home treatment.
Specialists can perform comprehensive evaluations including blood tests to identify underlying deficiencies, scalp biopsies if necessary, and trichoscopy to assess follicle health. Early intervention often yields better outcomes, as delayed treatment may result in permanent follicle damage in some cases. Professional guidance ensures appropriate treatment selection and monitoring for potential side effects or complications during the recovery process.

Recovery Expectations and Prevention Strategies
Understanding realistic recovery expectations and implementing preventive measures are crucial for managing post-COVID hair loss effectively. While the journey back to full hair restoration requires patience, most individuals can expect significant improvement with proper care and realistic timeline expectations.
What to Expect During Recovery
Hair regrowth following post-COVID telogen effluvium typically begins 3-6 months after the initial hair loss episode, with studies showing that approximately 85% of patients experience noticeable recovery within 12 months [13]. During the early recovery phase, patients first notice short hairs emerging from previously affected areas, often appearing as fine, baby-like strands that gradually increase in hair thickness over time. As hair grows at an average rate of half an inch per month, these new hairs require several months to achieve meaningful length and volume.
The recovery process occurs in distinct stages, beginning with the appearance of short hairs around the hairline and crown areas where loss was most pronounced. More hair follicles gradually return to their active growth phase, producing stronger, thicker strands with each growth cycle. Patients should understand that initial regrowth may appear different in texture or color compared to pre-illness hair, but these characteristics typically normalize as the follicles fully recover their function.
Long covid patients may experience extended recovery timelines, with some individuals requiring 18-24 months for complete restoration [14]. The quality and speed of regrowth often correlate with overall health status, nutritional support, and stress management during the recovery period. Patience remains essential, as premature concerns about slow progress can create additional stress that potentially delays the healing process.
Prevention Strategies for Future Episodes
Protecting against future hair loss episodes requires a comprehensive approach focused on immune system support and stress resilience. Maintaining optimal nutrition through a balanced diet rich in proteins, vitamins, and minerals provides essential building blocks for healthy hair follicle function. Regular exercise, adequate sleep, and stress management techniques such as meditation or yoga help regulate cortisol levels that can trigger telogen effluvium during future illnesses.
Early intervention strategies prove particularly valuable when facing subsequent health challenges. Recognizing early signs of systemic stress and implementing immediate supportive measures can minimize hair follicle disruption. This includes maintaining consistent sleep schedules, ensuring adequate hydration, and considering nutritional supplementation during illness recovery periods.
Building immune resilience through lifestyle modifications reduces the likelihood and severity of future post-viral hair loss episodes. Regular health monitoring, prompt treatment of infections, and maintaining strong social support networks contribute to overall stress reduction and improved recovery outcomes when health challenges arise.

Conclusion
COVID hair loss affects millions of individuals worldwide, representing one of the most common post-viral complications following infection. Understanding that this condition typically manifests as temporary hair loss provides crucial reassurance for those experiencing distressing changes in their scalp hair. The disruption to the normal hair cycle caused by viral infections creates a predictable pattern of hair loss that, while concerning, generally resolves with time and appropriate care.
Recovery requires patience, as hair growth occurs gradually over several months. The hair cycle must reset and stabilize before noticeable improvement becomes apparent. Most individuals experiencing post-viral hair loss can expect significant recovery within six to twelve months, though complete restoration may take longer in some cases.
Professional consultation becomes essential when hair loss persists beyond expected timeframes or appears more severe than typical temporary hair loss patterns. Doctors with a special interest in hair & scalp health can assess individual cases, rule out underlying conditions, and recommend targeted treatments when necessary. Early intervention often improves outcomes and provides peace of mind during the recovery process.
While covid hair loss remains a challenging experience, understanding its temporary nature and available treatment options empowers individuals to navigate this condition with confidence and appropriate medical support.
Frequently Asked Questions
Hair loss typically begins 2-4 months after COVID-19 infection, as this aligns with the natural hair growth cycle disruption caused by the stress of illness.
Most COVID-related hair loss is temporary. The majority of people see significant regrowth within 6-12 months, though full recovery may take up to 18 months in some cases.
While you cannot completely prevent post-viral hair loss, maintaining good nutrition, managing stress, and supporting your immune system may reduce severity and duration.
Topical minoxidil, stress management, proper nutrition, and gentle hair care are most effective. Severe cases may benefit from professional dermatological treatments.
References
- Guo J, Dai X, Wang H, et al. COVID-19-induced hair loss and its characteristics. Clin Exp Dermatol. 2021;46(7):1238-1242.
- Domínguez-Santás M, Haya-Martínez L, Fernández-Nieto D, et al. Acute telogen effluvium associated with SARS-CoV-2 infection. Australas J Dermatol. 2020;61(4):e434-e437.
- Trüeb RM, Dutra Rezende H, Gavazzoni Dias MFR. What can the hair tell us about COVID-19? Exp Dermatol. 2021;30(2):288-290.
- Dominguez-Santas M, Diaz-Guimaraens B, Fernandez-Nieto D. Acute telogen effluvium associated with SARS-CoV-2 infection. Australas J Dermatol. 2021;62(3):e282-e284.
- Rossi A, Magri F, Michelini S, et al. Investigation of cutaneous side effects of COVID-19 vaccines and of skin lesions COVID-19-related: a multicenter study. J Cosmet Dermatol. 2021;20(10):3100-3108.
- Rossi A, Magri F, Sernicola A, et al. Telogen effluvium after SARS-CoV-2 infection: a series of cases and possible pathogenetic mechanisms. Skin Appendage Disord. 2021;7(3):193-198.
- Mieczkowska K, Deutsch A, Borok J, et al. Telogen effluvium: a sequela of COVID-19. Int J Dermatol. 2021;60(1):122-124.
- Rossi A, Magri F, Sernicola A, et al. Telogen effluvium after SARS-CoV-2 infection: a series of cases and possible pathogenetic mechanisms. Skin Appendage Disord. 2022;8(1):35-41.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
- Gupta AK, Talukder M, Venkataraman M, Bamimore MA. Minoxidil: a comprehensive review. J Dermatolog Treat. 2022;33(4):1896-1906.
- Rossi A, Magri F, Sernicola A, et al. Telogen effluvium after SARS-CoV-2 infection: a series of cases and possible pathogenetic mechanisms. Skin Appendage Disord. 2021;7(5):365-370.
- Mieczkowska K, Deutsch A, Borok J, et al. Telogen effluvium: a sequela of COVID-19. Int J Dermatol. 2021;60(1):122-124.
- Rossi A, Magri F, Michelini S, et al. Investigation of the possible correlation between androgenetic alopecia and COVID-19. J Cosmet Dermatol. 2021;20(11):3608-3610.
- Bertolini M, Pirro F, Gandolfi G, et al. Hair Loss in Long COVID. Int J Trichology. 2021;13(5):190-194.